Services provided
Consultation Services
Electroencephalogram (EEG)
Video-EEG Monitoring
NCS (NERVE CONDUCTION STUDY)
EMG (ELECTROMYOGRAM)
VEP(VISUAL EVOKED POTENTIAL)
Brainstem Auditory Evoked Response(BAER)
Somatosensory Evoked Potential (SSEP)
AUTONOMIC TESTING(FIRST TIME ONLY CENTRE IN JHARKHAND)
CSF STUDY
Nerve and Muscle Biopsy
PHYSICAL MEDICINE & REHABILITATION
Dietary Services
Botulinum Neurotoxin Type A therapy
-
Consultation Services

The concept of medical consultation has grossly changed in recent times. The success of any consultation depends on how well the patient and doctor communicate with each other. There is now firm evidence linking the quality of this communication to clinical outcomes. We at Roy Neuro Care try to give “Care” to our patient by adopting the concept of “the dual focus” and “involving patients”
The dual focus—Patients are not exclusively physically ill or exclusively emotionally distressed. Often they are both. At the start of a consultation it is usually not possible to distinguish between these states. It is the doctor's task to listen actively to the patient's story, seeking and noticing evidence for both physical illness and emotional distress.
Involving patients—Changes in society and health care in the past decade have resulted in real changes in what people expect from their doctors and in how doctors view patients. In addition, greater emphasis has been placed on the reduction of risk factors, with attempts to persuade people to take preventive action and avoid risks to health. Many patients want more information than they are given. They also want to take some part in deciding about their treatment in the light of its chances of success and any side effects. Some patients, of course, do not wish to participate in decision making; they would prefer their doctor to decide on a single course of action and to advise them accordingly. The skill lies in achieving the correct balance for each patient.
There are several neurological disorders, and when we try to enlist diseases need to be dealt by a neurologist, the list is too long. However, here are a list of disorders in which a consultation from a neurologist may be necessary:
- Headache Disorders/ Migraine
- Seizure Disorders/ Epilepsy/ Loss of consciousness
- Stroke
- Parkinson's Disease
- Tremor of hands, legs or neck and other movement disorders
- Memory Problems/ Dementia (Alzheimer's Disease)
- Back and Neck Pain
- Painful Neuropathy
- Other Neuromuscular disorders
- Demyelinating Disorders of Brain
- Infections of Brain / spinal cord
-
Headache disorders/Migraine

Any slight change in quality and severity of your common daily headache should be taken seriously as it may be beginning of a Secondary headache include secondary causes of headache like tumors, infection, trauma, stroke etc.
Key facts
- Headache disorders are among the most common disorders of the nervous system.
- It has been estimated that almost half of the adult population have had a headache at least once within the last year.
- Headache disorders, which are characterized by recurrent headache, are associated with personal and societal burdens of pain, disability, damaged quality of life, and financial cost.
- Worldwide, a minority of people with headache disorders are diagnosed appropriately by a health-care provider.
- Headache has been underestimated, under-recognized and under-treated throughout the world.
What are headache disorders?
Headache disorders, characterized by recurrent headache, are among the most common disorders of the nervous system. Headache itself is a painful and disabling feature of a small number of primary headache disorders, namely migraine, tension-type headache, and cluster headache. Headache can also be caused by or occur secondarily to a long list of other conditions, the most common of which is medication-overuse headache.
How common are headache disorders?
Globally, it has been estimated that prevalence among adults of current headache disorder (symptomatic at least once within the last year) is about 50%. Half to three quarters of adults aged 18–65 years in the world have had headache in the last year and, among those individuals, 30% or more have reported migraine. Headache on 15 or more days every month affects 1.7–4% of the world’s adult population. Despite regional variations, headache disorders are a worldwide problem, affecting people of all ages, races, income levels and geographical areas.
What is the burden due to headache disorders?
Not only is headache painful, but it is also disabling. In the Global Burden of Disease Study, updated in 2013, migraine on its own was found to be the sixth highest cause worldwide of years lost due to disability (YLD). Headache disorders collectively were third highest.
Headache disorders impose a recognizable burden on sufferers including sometimes substantial personal suffering, impaired quality of life and financial cost. Repeated headache attacks, and often the constant fear of the next one, damage family life, social life and employment. The long-term effort of coping with a chronic headache disorder may also predispose the individual to other illnesses. For example, anxiety and depression are significantly more common in people with migraine than in healthy individuals.
Types of headache disorders
There are two types of headache disorders primary and secondary. Secondary headache include secondary causes of headache like tumors, infection, trauma, stroke etc. Primary headaches like migraine, tension-type headache and medication-overuse headache are of public health importance since they are responsible for high population levels of disability and ill-health.
Migraine
- A primary headache disorder.
- Migraine most often begins at puberty and most affects those aged between 35 and 45 years.
- It is more common in women, usually by a factor of about 2:1, because of hormonal influences.
- It is caused by the activation of a mechanism deep in the brain that leads to release of pain-producing inflammatory substances around the nerves and blood vessels of the head.
- Migraine is recurrent, often life-long, and characterized by recurring attacks.
HOW TO JOT DOWN YOUR MIGRAINE PATTERNS?
7 important items to list in your migraine diary
- 1- Date and time
- This is basic- always list the date, day of the week, and time when you first start noticing the beginnings of a migraine headache, including symptoms such as tiredness, elation, changes in appetite, strange scents, and migraine auras.
- Also, keep track of when your headache ended, and how long it took you to recuperate.
- 2- Rate the pain
- On a scale of one through ten, was this the worst headaches you’ve ever experienced, or was it on the usual pain threshold? Did your headache start at one side of the face and spread out, or was it confined to one specific area of your head?
- 3- Food
- There are hundreds of food items that may contribute to migraine headaches, so it’s important to always write down what you eat each day. Migraine triggers in food vary for each individual, so don’t compare your red-light foods to others who suffer from chronic migraine attacks.
- 4- Sleep
- Did you sleep in? Weekend headache is a common trigger for migraines, as it disturbs your body’s need for regularity. Take notes if you fall asleep for a nap in the afternoon, or wake up later than usual while on vacation.
- 5- Weather changes
- What was the weather like today? Was it very hot and humid? You may find that you’re more prone to migraines during certain seasonal changes. While you can’t avoid the weather, you can take measures to control symptoms that trigger migraine attacks. Keep the windows shut during pollen season, or run a humidifier in your office when the air is dry.
- 6- Physical activity
- Believe it or not, some migraine attacks are started by even mild physical exertion. “Exercise migraines” can also happen from coughing, strong bowel movements, sudden jerks of the head, or sexual intercourse.
- 7- Unusual headaches
- This may be the most crucial, yet most underappreciated detail to include in your migraine diary. Migraine attacks usually follow a pattern; migraines with aura are preceded by unusual visual disturbances, sudden fatigue, and increased sensitivity to bright lights, sounds, and scents.
- If you experience any out-of-the-ordinary headache symptoms, then keep track of all the details and speak to your doctor.
- 8- Medications and natural treatments
- Which migraine preventatives are you using, and how much? If you took over-the-counter or prescription pain relievers, then keep track of how many milligrams you consumed each day.
Tension-type headache (TTH)
- TTH is the most common primary headache disorder.
- Episodic TTH,occurring on fewer than 15 days per month, is reported by more than 70% of some populations.
- Chronic TTH, occurring on more than 15 days per month, affects 1-3% of adults.
- TTH often begins during the teenage years, affecting three women to every two men.
- Its mechanism may be stress-related or associated with musculoskeletal problems in the neck.
- Episodic TTH attacks usually last a few hours, but can persist for several days.
- Chronic TTH can be unremitting and is much more disabling than episodic TTH.
- This headache is described as pressure or tightness, often like a band around the head, sometimes spreading into or from the neck.
Cluster Headache (CH)
- A primary headache disorder.
- CH is relatively uncommon affecting fewer than 1 in 1000 adults, affecting six men to each woman.
- Most people developing CH are in their 20s or older.
- It is characterized by frequently recurring (up to several times a day), brief but extremely severe headache, usually focused in or around one eye, with tearing and redness of the eye, the nose runs or is blocked on the affected side and the eyelid may droop.
- CH has episodic and chronic forms.
Medication-overuse headache (MOH)
- MOH is caused by chronic and excessive use of medication to treat headache.
- MOH is the most common secondary headache disorder.
- It may affect up to 5% of some populations, women more than men.
- MOH occurs by definition on more days than not, is oppressive, persistent and often at its worst on awakening.
Social and economic burden of headache
Headache disorders are a public-health concern given the associated disability and financial costs to society. As headache disorders are most troublesome in the productive years (late teens to 50s), estimates of their financial cost to society – principally from lost working hours and reduced productivity – are massive. In the United Kingdom, for example, some 25 million working- or school-days are lost every year because of migraine alone; this financial cost may be matched by TTH and MOH combined. Headache is high among causes of consulting medical practitioners: one-third of all neurological consultations were for headache, in one survey.
Yet, many of those troubled by headache do not receive effective care. For example, in the United States of America and the United Kingdom, only half of those identified with migraine had seen a doctor for headache-related reasons in the previous 12 months, and only two-thirds had been correctly diagnosed. Most were solely reliant on over-the-counter medications.
Treatment
Appropriate treatment of headache disorders requires training of health professionals, accurate diagnosis and recognition of the conditions, appropriate treatment with cost-effective medications, simple lifestyle modifications, and patient education. The main classes of drugs to treat headache disorders include: analgesics, anti-emetics, specific anti-migraine medications, and prophylactic medications.
Barriers to effective care
Lack of knowledge among health-care providers is the principal clinical barrier. Worldwide, on average, only 4 hours of undergraduate medical education are dedicated to instruction on headache disorders. A large number of people with headache disorders are not diagnosed and treated: worldwide only 40% of those with migraine or TTH are professionally diagnosed, and only 10% of those with MOH.
Poor awareness extends to the general public. Headache disorders are not perceived by the public as serious since they are mostly episodic, do not cause death, and are not contagious. The low consultation rates in developed countries may indicate that many affected people are unaware that effective treatments exist. Half of people with headache disorders are estimated to be self-treating.
Many governments, seeking to constrain health-care costs, do not acknowledge the substantial burden of headache on society. They might not recognize that the direct costs of treating headache are small in comparison with the huge indirect-cost savings that might be made (eg, by reducing lost working days) if resources were allocated to treat headache disorders appropriately.
-
Seizure Disorders

In seizure disorders, the brain's electrical activity is periodically disturbed, resulting in some degree of temporary brain dysfunction.
- Many people have unusual sensations just before a seizure starts.
- Some seizures cause uncontrollable shaking and loss of consciousness, but more often, people simply stop moving or become unaware of what is happening.
- Doctors suspect the diagnosis based on symptoms, but imaging of the brain, blood tests, and electroencephalography (to record the brain’s electrical activity) are usually needed to identify the cause.
- If needed, drugs can usually help prevent seizures.
Normal brain function requires an orderly, organized, coordinated discharge of electrical impulses. Electrical impulses enable the brain to communicate with the spinal cord, nerves, and muscles as well as within itself. Seizures may result when the brain’s electrical activity is disrupted.
About 2% of adults have a seizure at some time during their life. Two thirds of these people never have another one. Seizure disorders commonly begin in early childhood or in late adulthood.
Types of seizures
Seizures may be described as follows:
- Epileptic: These seizures have no apparent trigger (that is, they are unprovoked), and they occur two or more times. One seizure is not considered epilepsy. Epileptic seizures are called a seizure disorder or epilepsy. What causes epileptic seizures is often unknown (called idiopathic epilepsy). But they may be caused by various brain disorders, such as structural abnormalities, strokes, or tumors. In such cases, they are called symptomatic epilepsy. Symptomatic epilepsy is most common among newborns and older people.
- Nonepileptic: These seizures are triggered (provoked) by a reversible disorder or a condition that irritates the brain, such as an infection, a stroke, a head injury, or a reaction to a drug. In children, a fever can trigger a nonepileptic seizure (called afebrile seizure). Certain mental disorders can cause symptoms that resemble seizures, called psychogenic nonepileptic seizures or pseudoseizures.
Causes
Which causes are most common depend on when seizures start:
- Before age 2: High fevers or temporary metabolic abnormalities, such as abnormal blood levels of sugar (glucose), calcium, magnesium, vitamin B6, or sodium, can trigger one or more seizures. Seizures do not occur once the fever or abnormality resolves. If the seizures recur without such triggers, the cause is likely to be an injury during birth, a birth defect, or ahereditary metabolic abnormality or brain disorder.
- 2 to 14 years: Often, the cause is unknown (see also Seizures in Children).
- Adults: A head injury, stroke, or tumor may damage the brain, causing a seizure. Alcohol withdrawal (caused by suddenly stopping drinking) is a common cause of seizures. However, in about half of people in this age group, the cause is unknown.
- Older adults: The cause may be a brain tumor or stroke.
Seizures with no identifiable cause are called idiopathic.
Conditions that irritate the brain—such as injuries, certain drugs, sleep deprivation, infections, fever—or that deprive the brain of oxygen or fuel—such as abnormal heart rhythms, a low level of oxygen in the blood, or a very low level of sugar in the blood (hypoglycemia)—can trigger a single seizure whether a person has a seizure disorder or not. A seizure that results from such a stimulus is called a provoked seizure (and thus is a nonepileptic seizure).
People with a seizure disorder are more likely to have a seizure when the following occur:
- They are under excess physical or emotional stress.
- They are intoxicated or deprived of sleep.
- They have suddenly stopped drinking or using sedatives.
Avoiding these conditions can help prevent seizures.
Rarely, seizures are triggered by repetitive sounds, flashing lights, video games, or even touching certain parts of the body. In such cases, the disorder is called reflex epilepsy.
Symptoms
An aura(unusual sensations) describes how a person feels before a seizure starts, or it may be part of a focal aware seizure that is just starting. An aura may include any of the following:
- Abnormal smells or tastes
- Butterflies in the stomach
- Feeling as if something has been experienced before even though it has not (called déjà vu) or the opposite feeling—something seems unfamiliar even though it is familiar in some way (called jamais vu)
- An intense feeling that a seizure is about to begin
Almost all seizures are relatively brief, lasting from a few seconds to a few minutes. Most seizures last 1 to 2 minutes.
Occasionally, seizures recur repeatedly, as occurs in status epilepticus.
Most people who have a seizure disorder look and behave normally between seizures.
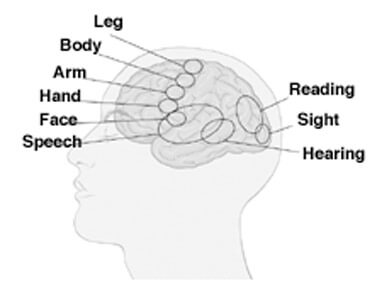
Symptoms of seizures vary depending on which area of the brain is affected by the abnormal electrical discharge, as in the following:
- An intensely pleasant or unpleasant taste if the part of the cerebrum called the insula is affected
- Visual hallucinations (seeing unformed images) if the occipital lobe is affected
- Inability to speak if the area that controls speech (located in the frontal lobe) is affected
- A convulsion (jerking and spasms of muscles throughout the body) if large areas on both sides of the brain are affected Seizures may be classified as
- Motor: Involving abnormal muscle contractions (such as jerking of a limb or convulsions)
- Nonmotor: Not involving abnormal muscle contractions
Other possible symptoms include numbness or tingling in a specific body part, brief episodes of unresponsiveness, loss of consciousness, and confusion. People may vomit if they lose consciousness. People may lose control of their muscles, bladder, or bowels. Some people bite their tongue.
Symptoms also vary depending on whether the seizure is
- Focal-onset (the seizure begins in one side of the brain)
- Generalized-onset (the seizure begins in both sides of the brain)
There are several types of focal and generalized seizures. Most people have only one type of seizure. Others have two or more types.
Some types of seizures may be focal or generalized:
- Atonic (involving loss of muscle tone)
- Clonic (involving rhythmic jerking of muscles)
- Tonic (involving stiffening of muscles)
- Myoclonic (involving sudden, lightning-like jerking of muscles)
- Epileptic (infantile) spasms and febrile seizures, which occur in children
Focal-onset seizures
In focal-onset seizures, the seizures begin in one side of the brain. These seizures are classified based on whether the person is aware during the seizure:
- Awareness is maintained (called focal aware seizures).
- Awareness is impaired (called focal impaired-awareness seizures).
Awareness refers to knowledge of self and environment. If awareness is impaired during any part of the seizure, the seizure is considered a focal impaired-awareness seizure. Doctors determine whether people remained aware during a seizure by asking them or, if a seizure is occurring, seeing if they respond when spoken to.
In focal aware seizures, abnormal electrical discharges begin in a small area of the brain and remain confined to that area. Because only a small area of the brain is affected, symptoms are related to the function controlled by that area. For example, if the small area of the brain that controls the right arm’s movements (in the left frontal lobe) is affected, the right arm may involuntarily be lifted up and jerk, and the head may turn toward the lifted arm. People are completely conscious and aware of the surroundings. A focal aware seizure may progress to a focal impaired-awareness seizure. Jacksonian seizures are a type of focal aware seizures. Symptoms start in one hand or foot, then move up the limb as the electrical activity spreads in the brain. People are completely aware of what is occurring during the seizure. Other focal aware seizures affect the face, then spread to an arm or sometimes a leg.
In focal impaired-awareness seizures, abnormal electrical discharges begin in a small area of the temporal lobe or frontal lobe and quickly spread to other nearby areas. The seizures usually begin with an aura, which lasts 1 to 2 minutes. During the aura, people start to lose touch with the surroundings.
During the seizure, awareness becomes impaired, but people do not become unconscious. People may do the following:
- Stare
- Chew or smack the lips involuntarily
- Move the hands, arms, and legs in strange, purposeless ways
- Utter meaningless sounds
- Not understand what other people are saying
- Resist help
Some people can converse, but their conversation lacks spontaneity, and the content is somewhat sparse. They may be confused and disoriented. This state may last for several minutes. Occasionally, people lash out if they are restrained.
Some people then recover fully. In others, the abnormal electrical discharge spreads to adjacent areas and to the other side of the brain, resulting in a generalized seizure. Generalized seizures that result from focal seizures are called focal to bilateral seizures. That is, they start in one side of the brain and spread to both sides.
Epilepsiapartialis continua is rare. Focal seizures occur every few seconds or minutes for days to years at a time. They typically affect an arm, a hand, or one side of the face. These seizures usually result from
- In adults: Localized brain damage (such as scarring due to a stroke)
- In children: Inflammation of the brain (as occurs in encephalitis and measles)
Generalized-onset seizures
In generalized-onset seizures, the seizure begins in both sides of the brain. Most generalized-onset seizures impair awareness. They often cause loss of consciousness and abnormal movements, usually immediately. Loss of consciousness may be brief or last a long time.
Generalized-onset seizures include the following types:
- Tonic-clonic seizures (formerly, called grand mal seizures)
- Clonic seizures
- Tonic seizures
- Atonic seizures
- Myoclonic seizures, including juvenile myoclonic epilepsy
- Epileptic (infantile) spasms
- Absence seizures
Most types of generalized seizures (such as tonic-clonic seizures) involve abnormal muscle contractions. Those that do not are called absence seizures.
In generalized tonic-clonic seizures, muscles contract (the tonic part), then rapidly alternate between contracting and relaxing (the clonic part). These seizures may be
- Generalized-onset (starting in both sides of the brain)
- Focal to bilateral (starting in one side of the brain and spreading to both sides)
In both types, consciousness is temporarily lost and a convulsion occurs when the abnormal discharges spread to both sides of the brain.
Generalized-onset seizures begin with abnormal discharges in a deep, central part of the brain and spread simultaneously to both sides of the brain. There is no aura. The seizure typically begins with an outcry. People then become unaware or lose consciousness. During generalized-onset seizures, people may do the following:
- Have severe muscle spasms and jerking throughout the body as muscles rapidly and repeatedly contract and relax
- Fall down
- Clench their teeth
- Bite their tongue (often occurs)
- Drool or froth at the mouth
- Lose control of the bladder and/or bowels
The seizures usually last 1 to 2 minutes. Afterward, some people have a headache, are temporarily confused, and feel extremely tired. These symptoms may last from minutes to hours. Most people do not remember what happened during the seizure.
Focal-to-bilateral tonic-clonic (grand mal) seizures usually begin with an abnormal electrical discharge in a small area of one side of the brain, resulting in a focal aware or focal impaired-awareness seizure. The discharge then quickly spreads to both sides of the brain, causing the entire brain to malfunction. Symptoms are similar to those of generalized-onset seizures.
Atonic seizures occur primarily in children. They are characterized by a brief but complete loss of muscle tone and consciousness. They cause children to fall to the ground, sometimes resulting in injury.
In clonic seizures, the limbs on both sides of the body and often head, neck, face, and trunk jerk rhythmically throughout the seizure. Clonic seizures usually occur in infants. They are much less common than tonic-clonic seizures.
Tonic seizures occur commonly during sleep, usually in children. Muscle tone increases abruptly or gradually, causing muscles to stiffen. The limbs and neck are often affected. Tonic seizures typically last only 10 to 15 seconds but can cause people, if standing, to fall to the ground. Most people do not lose consciousness. If seizures last longer, muscles may jerk a few times as the seizure ends.
Atypical absence seizures, atonic seizures, and tonic seizures usually occur as part of a severe form of epilepsy called Lennox-Gastaut syndrome, which begins before children are 4 years old.
Myoclonic seizures are characterized by quick jerks of one or several limbs or the trunk. The seizures are brief and do not cause loss of consciousness, but they may occur repetitively and may progress to a tonic-clonic seizure with loss of consciousness.
Juvenile myoclonic epilepsy typically begins during adolescence. Typically, seizures begin with quick jerks of both arms. About 90% of these seizures are followed by tonic-clonic seizures. Some people also have absence seizures. The seizures often occur when people awaken in the morning, especially if they are sleep-deprived. Drinking alcohol also makes these seizures more likely.
Absence seizures do not involve abnormal muscle contraction. They may be classified as
- Typical (petit mal)
- Atypical
Typical absence seizures usually begin in childhood, usually between the ages of 5 and 15 years, and do not continue into adulthood. However, adults occasionally have typical absence seizures. Unlike tonic-clonic seizures, absence seizures do not cause convulsions or other dramatic symptoms. People do not fall down, collapse, or move jerkily. Instead, they have episodes of staring with fluttering eyelids and sometimes twitching facial muscles. They typically lose consciousness, becoming completely unaware of their surroundings. These episodes last 10 to 30 seconds. People abruptly stop what they are doing and resume it just as abruptly. They experience no after-effects and do not know that a seizure has occurred. Without treatment, many people have several seizures a day. Seizures often occur when people are sitting quietly. Seizures rarely occur during exercise. Hyperventilation can trigger a seizure.
Atypical absence seizures differ from typical absence seizures as follows:
- They are less common.
- They last longer.
- Jerking and other movements are more pronounced.
- People are more aware of their surroundings.
Most people with atypical absence seizures have neurologic abnormalities or developmental delays. Atypical absence seizures usually continue into adulthood.
Status epilepticus
Convulsive status epilepticus is the most serious seizure disorder and is considered a medical emergency because the seizure does not stop. Electrical discharges occur throughout the brain, causing a generalized tonic-clonic seizure.
Convulsive status epilepticus is diagnosed when one or both of the following occur:
- A seizure lasts more than 5 minutes
- People do not completely regain consciousness between two or more seizures
People have convulsions with intense muscle contractions and often cannot breathe adequately. Body temperature increases. Without rapid treatment, the heart and brain can become overtaxed and permanently damaged, sometimes resulting in death.
Generalized convulsive status epilepticus has many causes, including injuring the head and abruptly stopping an antiseizure drug.
Nonconvulsive status epilepticus, another type of status epilepticus, does not cause convulsions. The seizures last 10 minutes or more. During the seizure, mental processes (including awareness) and/or behavior are affected. People may appear confused or spaced out. They may be unable to speak and may behave irrationally. Having nonconvulsive status epilepticus increases the risk of developing convulsive status epilepticus. This type of seizure requires prompt diagnosis and treatment.
Symptoms after a seizure
When a seizure stops, people may have a headache, sore muscles, unusual sensations, confusion, and profound fatigue. These after-effects are called the post-ictal state. In some people, one side of the body is weak after a seizure, and the weakness lasts longer than the seizure (a disorder called Todd paralysis).
Most people do not remember what happened during the seizure (a condition called post-ictal amnesia).
Complications
Seizures may have serious consequences. Intense, rapid muscle contractions can cause injuries, including broken bones. Sudden loss of consciousness can cause serious injury due to falls and accidents. People may have numerous seizures without incurring serious brain damage. However, seizures that recur and cause convulsions may eventually impair intelligence.
If seizures are not well-controlled, people may be unable to get a driver’s license. They may have difficulty keeping a job or getting insurance. They may be socially stigmatized. As a result, their quality of life may be substantially reduced.
If seizures are not completely controlled, people are two to three times more likely to die than those who do not have seizures.
A few people die suddenly for no apparent reason—a complication called sudden unexpected death in epilepsy. This disorder usually occurs at night or during sleep. Risk is highest for people who have frequent seizures, especially generalized tonic-clonic seizures.
Some interesting facts...
- Many types of seizures do not cause convulsions and loss of consciousness.
- Putting a spoon or other object in the mouth of someone having a convulsion can do more harm than good.
Symptoms
An aura (unusual sensations) describes how a person feels before a seizure starts, or it may be part of a focal aware seizure that is just starting. An aura may include any of the following:
- Abnormal smells or tastes
- Butterflies in the stomach
- Feeling as if something has been experienced before even though it has not (called déjà vu) or the opposite feeling—something seems unfamiliar even though it is familiar in some way (called jamais vu)
- An intense feeling that a seizure is about to begin
Almost all seizures are relatively brief, lasting from a few seconds to a few minutes. Most seizures last 1 to 2 minutes.
Occasionally, seizures recur repeatedly, as occurs in status epilepticus.
Most people who have a seizure disorder look and behave normally between seizures.
- An intensely pleasant or unpleasant taste if the part of the cerebrum called the insula is affected
- Visual hallucinations (seeing unformed images) if the occipital lobe is affected
- Inability to speak if the area that controls speech (located in the frontal lobe) is affected
- A convulsion (jerking and spasms of muscles throughout the body) if large areas on both sides of the brain are affected
Seizures may be classified as
- Motor: Involving abnormal muscle contractions (such as jerking of a limb or convulsions)
- Nonmotor: Not involving abnormal muscle contractions
Other possible symptoms include numbness or tingling in a specific body part, brief episodes of unresponsiveness, loss of consciousness, and confusion. People may vomit if they lose consciousness. People may lose control of their muscles, bladder, or bowels. Some people bite their tongue.
Symptoms also vary depending on whether the seizure is
- Focal-onset (the seizure begins in one side of the brain)
- Generalized-onset (the seizure begins in both sides of the brain)
There are several types of focal and generalized seizures. Most people have only one type of seizure. Others have two or more types.
Some types of seizures may be focal or generalized:
- Atonic (involving loss of muscle tone)
- Clonic (involving rhythmic jerking of muscles)
- Tonic (involving stiffening of muscles)
- Myoclonic (involving sudden, lightning-like jerking of muscles)
- Epileptic (infantile) spasms and febrile seizures, which occur in children
Focal-onset seizures
In focal-onset seizures, the seizures begin in one side of the brain. These seizures are classified based on whether the person is aware during the seizure:
- Awareness is maintained (called focal aware seizures).
- Awareness is impaired (called focal impaired-awareness seizures).
Awareness refers to knowledge of self and environment. If awareness is impaired during any part of the seizure, the seizure is considered a focal impaired-awareness seizure. Doctors determine whether people remained aware during a seizure by asking them or, if a seizure is occurring, seeing if they respond when spoken to.
In focal aware seizures, abnormal electrical discharges begin in a small area of the brain and remain confined to that area. Because only a small area of the brain is affected, symptoms are related to the function controlled by that area. For example, if the small area of the brain that controls the right arm’s movements (in the left frontal lobe) is affected, the right arm may involuntarily be lifted up and jerk, and the head may turn toward the lifted arm. People are completely conscious and aware of the surroundings. A focal aware seizure may progress to a focal impaired-awareness seizure.
Jacksonian seizures are a type of focal aware seizures. Symptoms start in one hand or foot, then move up the limb as the electrical activity spreads in the brain. People are completely aware of what is occurring during the seizure.
Other focal aware seizures affect the face, then spread to an arm or sometimes a leg.
In focal impaired-awareness seizures, abnormal electrical discharges begin in a small area of the temporal lobe or frontal lobe and quickly spread to other nearby areas. The seizures usually begin with an aura, which lasts 1 to 2 minutes. During the aura, people start to lose touch with the surroundings.
During the seizure, awareness becomes impaired, but people do not become unconscious. People may do the following:
- Stare
- Chew or smack the lips involuntarily
- Move the hands, arms, and legs in strange, purposeless ways
- Utter meaningless sounds
- Not understand what other people are saying
- Resist help
Some people can converse, but their conversation lacks spontaneity, and the content is somewhat sparse. They may be confused and disoriented. This state may last for several minutes. Occasionally, people lash out if they are restrained.
Some people then recover fully. In others, the abnormal electrical discharge spreads to adjacent areas and to the other side of the brain, resulting in a generalized seizure. Generalized seizures that result from focal seizures are called focal to bilateral seizures. That is, they start in one side of the brain and spread to both sides.
Epilepsiapartialis continua is rare. Focal seizures occur every few seconds or minutes for days to years at a time. They typically affect an arm, a hand, or one side of the face. These seizures usually result from
- In adults: Localized brain damage (such as scarring due to a stroke)
- In children: Inflammation of the brain (as occurs in encephalitis and measles)
Generalized-onset seizures
In generalized-onset seizures, the seizure begins in both sides of the brain. Most generalized-onset seizures impair awareness. They often cause loss of consciousness and abnormal movements, usually immediately. Loss of consciousness may be brief or last a long time.
Generalized-onset seizures include the following types:
- Tonic-clonic seizures (formerly, called grand mal seizures)
- Clonic seizures
- Tonic seizures
- Atonic seizures
- Myoclonic seizures, including juvenile myoclonic epilepsy
- Epileptic (infantile) spasms
- Absence seizures
Most types of generalized seizures (such as tonic-clonic seizures) involve abnormal muscle contractions. Those that do not are called absence seizures.
In generalized tonic-clonic seizures, muscles contract (the tonic part), then rapidly alternate between contracting and relaxing (the clonic part). These seizures may be
- Generalized-onset (starting in both sides of the brain)
- Focal to bilateral (starting in one side of the brain and spreading to both sides)
In both types, consciousness is temporarily lost and a convulsion occurs when the abnormal discharges spread to both sides of the brain.
Generalized-onset seizures begin with abnormal discharges in a deep, central part of the brain and spread simultaneously to both sides of the brain. There is no aura. The seizure typically begins with an outcry. People then become unaware or lose consciousness.
During generalized-onset seizures, people may do the following:
- Have severe muscle spasms and jerking throughout the body as muscles rapidly and repeatedly contract and relax
- Fall down
- Clench their teeth
- Bite their tongue (often occurs)
- Drool or froth at the mouth
- Lose control of the bladder and/or bowels
The seizures usually last 1 to 2 minutes. Afterward, some people have a headache, are temporarily confused, and feel extremely tired. These symptoms may last from minutes to hours. Most people do not remember what happened during the seizure
Focal-to-bilateral tonic-clonic (grand mal) seizures usually begin with an abnormal electrical discharge in a small area of one side of the brain, resulting in a focal aware or focal impaired-awareness seizure. The discharge then quickly spreads to both sides of the brain, causing the entire brain to malfunction. Symptoms are similar to those of generalized-onset seizures.
Atonic seizures occur primarily in children. They are characterized by a brief but complete loss of muscle tone and consciousness. They cause children to fall to the ground, sometimes resulting in injury.
In clonic seizures, the limbs on both sides of the body and often head, neck, face, and trunk jerk rhythmically throughout the seizure. Clonic seizures usually occur in infants. They are much less common than tonic-clonic seizures.
Tonic seizures occur commonly during sleep, usually in children. Muscle tone increases abruptly or gradually, causing muscles to stiffen. The limbs and neck are often affected. Tonic seizures typically last only 10 to 15 seconds but can cause people, if standing, to fall to the ground. Most people do not lose consciousness. If seizures last longer, muscles may jerk a few times as the seizure ends.
Atypical absence seizures, atonic seizures, and tonic seizures usually occur as part of a severe form of epilepsy called Lennox-Gastaut syndrome, which begins before children are 4 years old.
Myoclonic seizures are characterized by quick jerks of one or several limbs or the trunk. The seizures are brief and do not cause loss of consciousness, but they may occur repetitively and may progress to a tonic-clonic seizure with loss of consciousness.
Juvenile myoclonic epilepsy typically begins during adolescence. Typically, seizures begin with quick jerks of both arms. About 90% of these seizures are followed by tonic-clonic seizures. Some people also have absence seizures. The seizures often occur when people awaken in the morning, especially if they are sleep-deprived. Drinking alcohol also makes these seizures more likely.
Absence seizures do not involve abnormal muscle contraction. They may be classified as
- Typical (petit mal)
- Atypical
Typical absence seizures usually begin in childhood, usually between the ages of 5 and 15 years, and do not continue into adulthood. However, adults occasionally have typical absence seizures. Unlike tonic-clonic seizures, absence seizures do not cause convulsions or other dramatic symptoms. People do not fall down, collapse, or move jerkily. Instead, they have episodes of staring with fluttering eyelids and sometimes twitching facial muscles. They typically lose consciousness, becoming completely unaware of their surroundings. These episodes last 10 to 30 seconds. People abruptly stop what they are doing and resume it just as abruptly. They experience no after-effects and do not know that a seizure has occurred. Without treatment, many people have several seizures a day. Seizures often occur when people are sitting quietly. Seizures rarely occur during exercise. Hyperventilation can trigger a seizure.
Atypical absence seizures differ from typical absence seizures as follows:
- They are less common.
- They last longer.
- Jerking and other movements are more pronounced.
- People are more aware of their surroundings.
Most people with atypical absence seizures have neurologic abnormalities or developmental delays. Atypical absence seizures usually continue into adulthood.
Status Epilepticus
Convulsive status epilepticus is the most serious seizure disorder and is considered a medical emergency because the seizure does not stop. Electrical discharges occur throughout the brain, causing a generalized tonic-clonic seizure.
Convulsive status epilepticus is diagnosed when one or both of the following occur:
- A seizure lasts more than 5 minutes
- People do not completely regain consciousness between two or more seizures
People have convulsions with intense muscle contractions and often cannot breathe adequately. Body temperature increases. Without rapid treatment, the heart and brain can become overtaxed and permanently damaged, sometimes resulting in death.
Generalized convulsive status epilepticus has many causes, including injuring the head and abruptly stopping an antiseizure drug.
Nonconvulsive status epilepticus, another type of status epilepticus, does not cause convulsions. The seizures last 10 minutes or more. During the seizure, mental processes (including awareness) and/or behavior are affected. People may appear confused or spaced out. They may be unable to speak and may behave irrationally. Having nonconvulsive status epilepticus increases the risk of developing convulsive status epilepticus. This type of seizure requires prompt diagnosis and treatment.
Symptoms after a seizure
When a seizure stops, people may have a headache, sore muscles, unusual sensations, confusion, and profound fatigue. These after-effects are called the post-ictal state. In some people, one side of the body is weak after a seizure, and the weakness lasts longer than the seizure (a disorder called Todd paralysis).
Most people do not remember what happened during the seizure (a condition called post-ictal amnesia).
Complications
Seizures may have serious consequences. Intense, rapid muscle contractions can cause injuries, including broken bones. Sudden loss of consciousness can cause serious injury due to falls and accidents. People may have numerous seizures without incurring serious brain damage. However, seizures that recur and cause convulsions may eventually impair intelligence.
If seizures are not well-controlled, people may be unable to get a driver’s license. They may have difficulty keeping a job or getting insurance. They may be socially stigmatized. As a result, their quality of life may be substantially reduced.
If seizures are not completely controlled, people are two to three times more likely to die than those who do not have seizures.
A few people die suddenly for no apparent reason—a complication called sudden unexpected death in epilepsy. This disorder usually occurs at night or during sleep. Risk is highest for people who have frequent seizures, especially generalized tonic-clonic seizures.
Some interesting facts...
- Many types of seizures do not cause convulsions and loss of consciousness.
- Putting a spoon or other object in the mouth of someone having a convulsion can do more harm than good.
-
Diagnosis

- A doctor's evaluation
- If the person has never had a seizure before, blood and other tests, imaging of the brain, and usually electroencephalography
- If a seizure disorder has already been diagnosed, usually blood tests to measure levels of antiseizure drugs
Doctors diagnose a seizure disorder when people have at least two unprovoked seizures that occur at different times. The diagnosis is based on symptoms and the observations of eyewitnesses. Symptoms that suggest a seizure include loss of consciousness, muscle spasms that shake the body, loss of bladder control, sudden confusion, and inability to pay attention. However, seizures cause such symptoms much less often than most people think. A brief loss of consciousness is more likely to be fainting (syncope) than a seizure.
People are usually evaluated in an emergency department. If a seizure disorder has already been diagnosed and people have completely recovered, they may be evaluated in a doctor’s office.
History and physical examination
An eyewitness report of the episode can be very helpful to doctors. An eyewitness can describe exactly what happened, whereas people who have an episode usually cannot. Doctors need to have an accurate description, including the following:
- How fast the episode started
- Whether it involved abnormal muscle movements (such as spasms of the head, neck, or facial muscles), tongue biting, drooling, loss of bladder or bowel control, or muscle stiffening
- How long it lasted
- How quickly the person recovered
A quick recovery suggests fainting rather than a seizure. Confusion that lasts for many minutes to hours after consciousness is regained suggests a seizure.
Although eyewitnesses may be too frightened during the seizure to remember all details, whatever they can remember can help. If possible, how long a seizure lasts should be timed with a watch or other device. Seizures that last only 1 or 2 minutes can seem to go on forever.
Doctors also need to know what people experienced before the episode: whether they had a premonition or warning that something unusual was about to happen and whether anything, such as certain sounds or flashing lights, seemed to trigger the episode.
Doctors ask people about possible causes of seizures, such as the following:
- Whether people have had a disorder that can cause seizures (such as a brain infection) or a head injury
- Which drugs (including alcohol) they are taking or have recently stopped
- For people who are taking drugs to control seizures, whether they are taking the drugs as directed
- Whether they are getting enough sleep (not getting enough sleep can make seizures more likely to occur in some people)
A thorough physical examination is done. It may provide clues to the cause of the symptoms.
Testing
Once a seizure is diagnosed, more tests are usually needed to identify the cause.
People known to have a seizure disorder may not need tests, except for a blood test to measure the levels of the antiseizure drugs they are taking.
In other people, blood tests are often done to measure the levels of substances such as sugar, calcium, sodium, and magnesium and to determine whether the liver and kidneys are functioning normally. A sample of urine may be analyzed to check for recreational drugs that may not be reported. Such drugs can trigger a seizure.
Electrocardiography may be done to check for an abnormal heart rhythm. Because an abnormal heart rhythm can greatly reduce blood flow (and therefore oxygen supply) to the brain, it can trigger loss of consciousness and occasionally a seizure or symptoms that resemble a seizure.
Imaging of the brain is usually done promptly to check for bleeding or a stroke. Typically, computed tomography (CT) is done, but magnetic resonance imaging (MRI) may be done. Both tests can identify brain abnormalities that could be causing seizures. MRI provides clearer, more detailed images of the brain tissue, but it is not always readily available.
If doctors suspect a brain infection such as meningitis or encephalitis, a spinal tap (lumbar puncture) is usually done.
Electroencephalography (EEG) can help confirm the diagnosis. EEG is a painless, safe procedure that records electrical activity in the brain. Doctors examine the recording (electroencephalogram) for evidence of abnormal electrical discharges. Because the recording time is limited, EEG can miss abnormalities, and results may be normal, even in people who have a seizure disorder. EEG is sometimes scheduled after people have been deprived of sleep for 18 to 24 hours because lack of sleep makes abnormal discharges more likely to occur.
Brain Activity During a Seizure
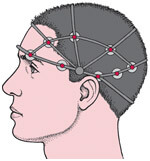 An electroencephalogram (an EEG) is a recording of the brain’s electrical activity. The procedure is simple and painless. About 20 small adhesive electrodes are placed on the scalp, and the brain’s activity is recorded under normal conditions. Then the person is exposed to various stimuli, such as bright or flashing lights, to try to provoke a seizure. During a seizure, electrical activity in the brain accelerates, producing a jagged wave pattern. Such recordings of brain waves help identify a seizure disorder. Different types of seizures have different wave patterns.
An electroencephalogram (an EEG) is a recording of the brain’s electrical activity. The procedure is simple and painless. About 20 small adhesive electrodes are placed on the scalp, and the brain’s activity is recorded under normal conditions. Then the person is exposed to various stimuli, such as bright or flashing lights, to try to provoke a seizure. During a seizure, electrical activity in the brain accelerates, producing a jagged wave pattern. Such recordings of brain waves help identify a seizure disorder. Different types of seizures have different wave patterns. 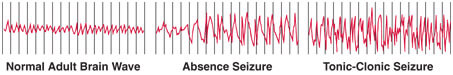
EEG may be repeated because when done a second or even a third time, it may detect the cause, which was missed the first time the test was done.
If the diagnosis is still uncertain, specialized tests, such as video-EEG monitoring, can be done at an epilepsy center.
For video-EEG monitoring, people are admitted to a hospital for 2 to 7 days, and EEG is done while they are video-taped. If people are taking an antiseizure drug, it is often stopped to increase the likelihood of a seizure. If a seizure occurs, doctors compare the EEG recording with the video recording of the seizure. They may then be able to identify the type of seizure and the area of the brain where the seizure began.
Ambulatory EEG enables doctors to record brain activity for days at a time—while people are at home. It may be useful if seizures recur in people who cannot be admitted to the hospital for a long time.
Prognosis
With treatment, one third of people with epilepsy are free from seizures, and most become seizure-free shortly after starting treatment. In another third, seizures recur less than half as often as they did before treatment. If seizures are well-controlled with drugs, about 60 to 70% of people can eventually stop taking antiseizure drugs and remain seizure-free.
Epileptic seizures are considered resolved when people have been seizure-free for 10 years and have not taken antiseizure drugs for the last 5 years of that time period.
Treatment
- Elimination of the cause if possible
- General measures
- Drugs to control seizures
- Sometimes surgery or other procedures if drugs are ineffective
If the cause of the seizures can be identified and eliminated, no additional treatment is necessary. For example, if a low blood sugar (glucose) level (hypoglycemia) caused the seizure, glucose is given, and the disorder causing the low level is treated. Other treatable causes include an infection, certain tumors, and an abnormal sodium level.
If the cause cannot be eliminated, general measures plus drugs are usually sufficient to treat seizure disorders. If drugs are ineffective, surgery may be recommended.
General measures
Exercise is usually recommended and social activities are encouraged. However, people who have a seizure disorder may have to make some adjustments. For example, they may be advised to do the following:
- Eliminate or limit their consumption of alcoholic beverages
- Not use recreational drugs
- Refrain from activities in which a sudden loss of consciousness could result in serious injury, such as bathing in a bathtub, climbing, swimming, or operating power tools
After seizures are controlled (typically for at least 6 months), they can do these activities if adequate precautions are taken. For example, they should swim only when lifeguards are present.
In most states, laws prohibit people with a seizure disorder from driving until they have been free of seizures for at least 6 months to 1 year.
A family member or close friend and coworkers should be trained to help if a seizure occurs. Attempting to put an object (such as a spoon) in the person’s mouth to protect the person’s tongue should not be tried. Such efforts can do more harm than good. The teeth may be damaged, or the person may bite the helper unintentionally as the jaw muscles contract. However, helpers should do the following during a seizure:
- Protect the person from falling
- Loosen clothing around the neck
- Place a pillow under the head
- Roll the person over to one side
If a pillow is unavailable, helpers can put their foot or place an item of clothing under the person’s head.
People who lose consciousness should be rolled onto one side to ease breathing and help prevent them from inhaling vomit or saliva. Inhaling vomit or saliva can lead to aspiration pneumonia (a lung infection caused by inhaling saliva, stomach contents, or both).
People who have had a seizure should not be left alone until they have awakened completely, are no longer confused, and can move about normally. Usually, their doctor should be notified.
Antiseizure drugs
Antiseizure drugs (also called anticonvulsants or antiepileptic drugs) reduce the risk of having another seizure. Usually, they are prescribed only if people have had more than one seizure and if reversible causes, such as low blood sugar, have been ruled out or completely corrected. Antiseizure drugs are usually not prescribed when people have had only one generalized seizure.
Most antiseizure drugs are taken by mouth.
Antiseizure drugs can completely stop seizures in about one third of people who have them and greatly reduce the frequency of seizures in another third. Almost two thirds of people who respond to antiseizure drugs can eventually stop taking them without having a relapse. However, if antiseizure drugs are ineffective, people are referred to a seizure center and evaluated for surgery.
There are many different types of antiseizure drugs. Which one is effective depends on the type of seizure and other factors. For most people, taking one antiseizure drug, usually the first or second one tried, controls seizures. If seizures recur, different antiseizure drugs are tried. In such cases, determining which drug is effective may take several months. Some people have to take several drugs, which increases the risk of side effects. Some antiseizure drugs are not used alone but only with other antiseizure drugs.
Doctors take care to determine the appropriate dose for each person. The best dose is the smallest dose that stops all seizures while having the fewest side effects. Doctors ask people about side effects, then adjust the dose if needed. Sometimes doctors also measure the level of antiseizure drug in the blood.
Antiseizure drugs should be taken just as prescribed. People who take drugs to control seizures should see a doctor regularly for dose adjustment and should always wear a medical alert bracelet inscribed with the type of seizure disorder and the drug being taken.
Antiseizure drugs can interfere with the effectiveness of other drugs, and vice versa. Consequently, people should make sure their doctor knows all the drugs they are taking before they start taking antiseizure drugs. They should also talk to their doctor and possibly their pharmacist before they start taking any other drugs, including over-the-counter drugs.
After seizures are controlled, people take the antiseizure drug until they have been seizure-free for at least 2 years. Then, the dose of the drug may be decreased gradually, and the drug eventually stopped. If a seizure recurs after the antiseizure drug is stopped, people may have to take an antiseizure drug indefinitely. Seizures usually recur within 2 years if they are going to.
Seizures are more likely to recur in people who have had any of the following:
- A seizure disorder since childhood
- The need to take more than one antiseizure drug to be seizure-free
- Seizures while taking an antiseizure drug
- Focal seizures or myoclonic seizures
- Abnormal EEG results within the previous year
- Structural damage to the brain—for example, by a stroke or tumor
Antiseizure drugs, although very effective, may have side effects. Many cause drowsiness, but some may make children hyperactive. For many antiseizure drugs, blood tests are done periodically to determine whether the drug is impairing kidney or liver function or reducing the number of blood cells. People taking antiseizure drugs should be aware of possible side effects and should consult their doctor at the first sign of side effects.
For women who have a seizure disorder and are pregnant, taking an antiseizure drug increases the risk of miscarrying or of having a baby with a birth defect of the spinal cord, spine, or brain (neural tube defect—see table Some Drugs That Can Cause Problems During Pregnancy). However, stopping the antiseizure drug may be more harmful to the woman and the baby. Having a generalized seizure during pregnancy can injure or kill the fetus. Consequently, continuing to take an antiseizure drug is usually recommended (see Seizure Disorders During Pregnancy). All women who are of childbearing age and taking an antiseizure drug should take folate supplements to reduce the risk of having a baby with a birth defect.
All women who are of childbearing age and taking an antiseizure drug should take folate supplements to reduce the risk of having a baby with a birth defect.
Emergency treatment
Emergency treatment to stop the seizures is required for
- Status epilepticus
- Seizures that last more than 5 minutes
Large doses of one or more antiseizure drugs (often starting with a benzodiazepine, such as lorazepam) are given intravenously as quickly as possible to stop the seizure. The sooner antiseizure drugs are started, the better and the more easily seizures are controlled.
Measures to prevent injuries are taken during the prolonged seizure. People are monitored closely to make sure breathing is adequate. If it is not, a tube is inserted to help with breathing—a procedure called intubation.
If seizures persist, a general anesthetic is given to stop them.
Surgery
If people continue to have seizures while taking two or more antiseizure drugs or if they cannot tolerate side effects of the drugs, brain surgery may be done. These people are tested at specialized epilepsy centers to determine whether surgery can help. Testing may include MRI of the brain, video-EEG monitoring, and the following:
- Functional MRI: To determine which areas in the brain are causing seizures (called seizure foci)
- Single-photon emission CT (SPECT): To check for areas with increased blood flow around the time of a seizure, which may indicate which areas in the brain are causing seizures
- EEG combined with magnets used for imaging (magnetic source imaging): Also to help determine which areas in the brain are causing seizures
If a defect in the brain (such as a scar) can be identified as the cause and is confined to a small area, surgically removing that area can eliminate seizures in up to 60% of people, or surgery may reduce the severity and frequency of seizures.
Surgically cutting the nerve fibers that connect the two sides of the brain (corpus callosum) may help people who have seizures that originate in several areas of the brain or that spread to all parts of the brain very quickly. This procedure usually has no appreciable side effects. However, even if surgery reduces the frequency and severity of seizures, many people need to continue to take antiseizure drugs. However, they can usually take lower doses or fewer drugs.
Before and after surgery, a psychologic and neurologic evaluation may be done to determine how well the brain is functioning.
If people cannot undergo these surgical procedures, other procedures, such as stimulation of the vagus nerve or brain, may be done.
Stimulation of the vagus nerve
Electrical stimulation of the 10th cranial nerve (vagus nerve) can reduce the number of focal-onset seizures by more than one half in about 40% of people who have focal-onset seizures. This treatment is used when seizures continue despite use of antiseizure drugs and when surgery is not a possibility.
The vagus nerve is thought to have indirect connections to areas of the brain often involved in causing seizures.
For this procedure, a device that looks like a heart pacemaker (vagus nerve stimulator) is implanted under the left collarbone and is connected to the vagus nerve in the neck with a wire that runs under the skin. The device causes a small bulge under the skin. The operation is done on an outpatient basis and takes about 1 to 2 hours.
The device is programmed to periodically stimulate the vagus nerve. Also, people are given a magnet, which they can use to stimulate the vagus nerve when they sense that a seizure is about to begin. Vagus nerve stimulation is used in addition to antiseizure drugs.
Side effects of vagal nerve stimulation include hoarseness, cough, and deepening of the voice when the nerve is stimulated.
Stimulation of the brain
The responsive neurostimulation system is a device that looks like a heart pacemaker. It is implanted within the skull. The device is connected by wires to one or two areas in the brain that are causing the seizures. This system monitors the brain's electrical activity. When it detects unusual electrical activity, it stimulates the areas of the brain that are causing the seizures. The aim is to restore normal electrical activity in the brain before a seizure can occur.
The responsive neurostimulation system is used in addition to antiseizure drugs. It is used when adults have focal-onset seizures that are not controlled by drugs. It can reduce the frequency of seizures in these people.
Surgery to implant the system requires general anesthesia and typically takes 2 to 4 hours. Many people can go home the next day. Some need to stay in the hospital for up to 3 days. Many people can return to their daily activities within a few days and return to work in 2 to 4 weeks.
People cannot feel the device or the stimulation, and the device can be removed if needed.
-
Stroke

“Stroke is a medical emergency. It is important to understand that management should be started as soon as possible because as each minute passes millions of neurons continue to die which can be irreversible.”
Stroke is one of the leading causes of death and disability in India. A stroke is the rapid loss of brain functions due to disturbance of blood vessels of the brain.
There are two major types of stroke:
- Ischemic stroke
- Hemorrhagic stroke
Ischemic stroke occurs when a blood vessel that supplies blood to the brain is blocked by a blood clot. A hemorrhagic stroke occurs when a blood vessel in part of the brain becomes weak and bursts open, causing blood to leak into the brain. This results in death of the brain cells due to lack of oxygen and glucose.
Within minutes the affected area of brain becomes nonfunctional, resulting in the inability to move one or more limbs, inability to understand or speak or inability to see one side of visual field. A stroke does not discriminate amongst its victims; it affects people of any age group, social status and gender. Though stroke symptoms may not be as painful or dramatic as a heart attack, brain stroke can be just as life-threatening or debilitating. Stroke is a medical emergency.
SYMPTOMS OF STROKE
The symptoms of stroke depend on which part of the brain is affected. The most common symptoms include:
- Sudden numbness or weakness of face, leg or arm, precisely on one side of the body.
- Loss of vision or blurred vision in one or both eyes.
- Loss of speech or difficulty in understanding others
- Sudden confusion or loss of memory.
- Loss of balance and trouble walking.
- Difficulty in swallowing.
- Sudden severe headache with no known cause.
- Severe headache
- Loss of consciousness
- Seizures
Stroke: Management
Stroke is a medical emergency. It is important to understand that management should be started as soon as possible because as each minute passes millions of neurons continue to die which can be irreversible. So, irrespective of type of stroke (ischemic or hemorrhagic treatment should be started as soon as possible. Initial 1-2 weeks is the most critical time during which patients deteriorate hence it is prudent to hospitalize patients during that period. Rehabilitation is the most important aspect as far as long term improvement from stroke is concerned.
Stroke: Rehabilitation Services
After a stroke, rehabilitation programs are critical in helping patients regain lost skills, relearn tasks, and work to be independent again.
Stroke Rehabilitation
What is stroke rehabilitation?
After hospitalization for stroke, many patients still have problems with physical, speech, and mental functions. Rehabilitation for these problems can be provided in a variety of settings. Rehabilitation programs are critical in helping patients regain lost skills, relearn tasks, and work to be independent again. In many cases, there is great potential for the brain to recover. With diligent rehabilitation, these prospects can get even better. Even if major neurological deficits do not improve, the patients’ functioning can improve as they learn ways to compensate for their problems.
Some factors that play a role in success of stroke rehabilitation are:
- The extent of the brain injury. The less severe the injury, the better the chances for recovery.
- The stroke survivor's attitude. A survivor's positive attitude can help him or her cope with difficult times and focus on getting better.
- Family support. A stroke survivor's family can be the most important form of support during rehabilitation. Family members can reassure stroke survivors that they're wanted, needed, and still important to the family.
- Time until start of rehabilitation. Rehabilitation must begin as soon after the stroke as possible. Even simple tasks such as exercising paralyzed muscles and turning the person in bed should begin very soon after the stroke. Stroke rehabilitation is most successful when it is a team effort. The stroke survivor and his or her family must work together with the doctor, nurse, and other rehabilitation specialists.
What happens after the stroke patient leaves the hospital?
Stroke rehabilitation is provided in a number of settings. Doctors, therapists, and case managers will determine what setting would provide the most appropriate treatment based primarily on the stroke disability and prognosis for improvement. Sayings like “no pain – no gain” and “use it or lose it” do not apply to stroke patients. More exercise is not necessarily better.
A safe and effective rehabilitation program allows patients to recover at a pace that fits their needs and abilities. Patients usually move among various levels of care during their recovery. Deciding on the right setting for rehabilitation involves many elements:
- The severity and unique characteristics of the physical problems caused by the stroke
- The presence of other medical conditions like arthritis, kidney disease, or heart disease
- Availability and location of family and friends
- Insurance coverage for rehabilitation services
What are the choices for stroke rehabilitation?
Acute rehabilitation
Three or more hours of therapy are provided five days a week, and sometimes over the weekend. Doctors may visit the patient five or more days a week. Patients at this level of care must demonstrate the ability to tolerate and benefit from intensive exercise and training.
Subacute or skilled nursing rehabilitation
In this type of rehabilitation, one or two hours of rehabilitation treatment are provided five days a week. Patients in this setting are often recovering from difficult medical problems, and are able to tolerate a moderate pace of exercise. Doctors supervise the medical and rehabilitative care, and visit the patient as needed, usually three times a week.
Outpatient rehabilitation
This means that the patient lives at home and travels two or three times a week to a rehabilitation facility for a few hours of treatment. Usually, family members drive patients to their treatments. Therapists can do a lot more in the facility than they can do in the patient’s home.
Rehabilitation in the home
This kind of rehabilitation usually is for homebound patients with very mild problems and extensive family support. Members of the therapy team come to the home of the patient, usually for 2 or 3 hours of therapy per week. Simple therapy services are provided.
Long-term acute care (LTAC) hospital rehabilitation
These rehabilitation services are provided in special hospital units that are designed to care for patients with major medical problems requiring intense treatment (patients that require ventilators for breathing, dialysis, drugs that support heart function). Doctors visit the patient frequently.
Nursing home restorative care
This kind of care is the least intensive level of rehabilitation care in an institutional setting. Patients participate in an exercise program a few hours a week, generally in a group setting.
How long does rehabilitation last?
Stroke rehabilitation takes time. Each advance in a patient’s skills and condition is a victory, and over time these small victories start to add up. For persons receiving rehabilitation services in an acute, subacute, skilled, LTAC or nursing home setting, the period of treatment often lasts from two to four weeks. After this, many patients can return home and engage therapy services over several months as they continue to recover.
Is the family involved?
Yes. The time that rehabilitation specialists spend with the patient in rehabilitation is just a “blink of the eye” in that patient’s lifetime. Family and friends' active involvement in the patient's rehabilitation process helps the patient achieve success. The patient’s loved ones can help specialists understand what the patient was like before the stroke and help plan for the best outcome after the patient goes home
-
Parkinson's disease

“The importance of recognizing early symptoms
Many people think that the early signs of Parkinson's are normal signs of aging. For this reason, they may not seek help.
However, treatment is more likely to be effective if a person takes it early in the development of PD. For this reason, it is important to get an early diagnosis if possible.”Parkinson's disease is a movement disorder. It affects the nervous system, and symptoms become worse over time.
The National Institutes of Health (NIH) note that, in the United States, around 50,000 peoplereceive a diagnosis of Parkinson's disease(PD) each year, and around half a million people are living with the condition.
Read on to find out more about this condition, the early signs, and what causes it.
What is Parkinson's disease?
The symptoms of PD develop gradually. They often start with a slight tremor in one hand and a feeling of stiffness in the body. Most of the symptoms result from a fall in dopamine levels in the brain.One study, based in France, found in 2015 that men are 50 percent more likely to develop PD than women overall, but the risk for women appears to increase with ageing most people, symptoms appear at the age of 60 years or over. However in 5–10 percent of cases they appear earlier. When PD develops before the age of 50 years, this is called "early onset" PD. Over time, other symptoms develop, and some people will have dementia.
Early signs
Here are some early signs of PD:
- Movement: There may be a tremor in the hands.
- Coordination: A reduced sense of coordination and balance can cause people to drop items they are holding. They may be more likely to fall.
- Gait: The person's posture may change, so that they lean forward slightly, as if they were hurrying. They may also develop a shuffling gait.
- Facial expression: This can become fixed, due to changes in the nerves that control facial muscles.
- Voice: There may be a tremor in the voice, or the person may speak more softly than before.
- Handwriting: This may become more cramped and smaller.
- Sense of smell: A loss of sense of smell can be an early sign.
- Sleep problems: These are a feature of Parkinson's, and they may be an early sign. Restless legs may contribute to this.
Other common symptoms include:
- mood changes, including depression
- difficulty chewing and swallowing
- problems with urination
- constipation
- skin problems
- sleep problems
REM sleep disorder: Authors of a study published in 2015 describe another neurological condition, REM sleep disorder, as a "powerful predictor" for PD and some other neurological conditions.
The importance of recognizing early symptoms
Many people think that the early signs of Parkinson's are normal signs of aging. For this reason, they may not seek help.
However, treatment is more likely to be effective if a person takes it early in the development of PD. For this reason, it is important to get an early diagnosis if possible.
If treatment does not start until the person has clear symptoms, it will not be as effective.
Moreover, a number of other conditions can have similar symptoms.
These include:
- drug-induced Parkinsonism
- head trauma
- encephalitis
- stroke
- Lewy body dementia
- corticobasal degeneration
- multiple system atrophy
- progressive supranuclear palsy
The similarity to other conditions can make it hard for doctors to diagnose Parkinson's disease in the early stages.
Movement symptoms may start on one side of the body and gradually affect both sides.
What is Parkinsonism?
Parkinsonism refers to a syndrome that has similar signs and symptoms to PD, but it is not the same thing. Click here to find out more.
Causes and risk factors
Scientists are not sure what causes PD. It happens when nerve cells die in the brain.
“If a person with Parkinson's also has changes known as Lewy bodies in the brain, they can develop dementia.”
Low dopamine levels: Scientists have linked low or falling levels of dopamine, a neurotransmitter, with PD. This happens when cells that produce dopamine die in the brain.
Dopamine plays a role in sending messages to the part of the brain that controls movement and coordination. Low dopamine levels can make it harder for people to control their movements.
As dopamine levels fall in a person with PD, their symptoms gradually become more severe.
Low norepinephrine levels: Norepinephrine, another neurotransmitter, is important for controlling many automatic body functions, such as the circulation of the blood.
In PD, the nerve endings that produce this neurotransmitter die. This may explain why people with PD experience not only movement problems but also fatigue, constipation, and orthostatic hypotension, when blood pressure changes on standing up, leading to light-headedness.
Lewy bodies: A person with PD may have clumps of protein in their brain known as Lewy bodies. Lewy body dementia is a different condition, but it has links with PD.
Genetic factors: Sometimes, PD appears to run in families, but it is not always hereditary. Researchers are trying to identify specific genetic factors that may lead to PD, but it appears that not one but a number of factors are responsible.
For this reason, they suspect that a combination for genetic and environmental factors may lead to the condition.
Possible environmental factors could include exposure to toxins, such as pesticides, solvents, metals, and other pollutants.
Autoimmune factors: Scientists reported in JAMA in 2017 that they had found evidence of a possible genetic link between PD and autoimmune conditions, such as rheumatoid arthritis.
In 2018, researchers investigating health records in Taiwan found that people with autoimmune rheumatic diseases (ARD) had a 1.37-higher chance of also having PD than people without ARD.
Prevention
“Using appropriate protection when using pesticides and other toxins may help reduce the risk of PD.”
It is not possible to prevent Parkinson's disease, but research has shown that some lifelong habits may help to reduce the risk.
Turmeric: This spice contains curcumin, an antioxidant ingredient. It may help to prevent the clumping of a protein involved in Parkinson's disease, at least one laboratory study has found.
Flavonoids: Consuming another type of antioxidant — flavonoids — may lower the risk of developing Parkinson's disease, according to research. Flavonoids are present in berries, apples, some vegetables, tea, and red grapes.
Avoiding reheated cooking oils: Scientists have linked toxic chemicals, known as aldehydes, to Parkinson's, Alzheimer's and other neurodegenerative diseases, and some cancers.
Heating certain oils — such as sunflower oil — to a certain temperature, and then using them again can cause aldehydes to occur in those oils.
Avoiding toxins: Exposure to herbicides, pesticides, and other toxins may increase the risk of neurological diseases such as PD. People should take precautions when using these types of product, for example, by using protective clothing.
Takeaway
Parkinson's disease is a lifelong condition that involves neurological changes in the body. These changes can make it harder for a person to function in daily life. However, medications and other types of therapy are available for treating PD and reducing the symptoms.
Current treatment can relieve symptoms, but scientists hope that gene therapy or stem cell therapy will one day be able to do more than this, and restore function that the person has already lost.
Tremor of hands, legs or neck and other movement disorders
- Essential Tremor — Essential tremor (ET) is the most common movement disorder. It is a progressive, often inherited disorder that usually begins in later adulthood. Patients with ET typically experience tremors when the arms are held up and when the hands are being used for activities like eating, drinking or writing.
- Dystonic tremor-Dystonic tremor is a type of tremor which occurs in conjunction with dystonia, a neurological disorder where incorrect messages from the brain cause muscles to be over-active resulting abnormal postures or unwanted movement. Dystonic tremorusually appears in young adulthood or mid-life.
- Ataxia — Persons who are diagnosed with ataxia experience a failure of muscle control in their arms and legs which may result in a lack of balance, coordination, and possibly a disturbance in gait. Ataxia may affect the fingers, hands, arms, legs, body, speech, and even eye movements.
- Dystonia — Dystonia is a neurological condition with a very broad range of manifestations including posturing of a particular body part. The basic underlying problem involves over-activity of the main muscles needed for a movement, extra activation of other muscles that are not needed for the movement, and simultaneous activation of muscles that work against each other.
-
Dementia and Alziemer’s disease

What Is Dementia?
Dementia is a general term for a decline in mental ability severe enough to interfere with daily life. Memory loss is an example. Alzheimer's is the most common type of dementia.
About dementia
Dementia is not a specific disease. It's an overall term that describes a group of symptoms associated with a decline in memory or other thinking skills severe enough to reduce a person's ability to perform everyday activities. Alzheimer's disease accounts for 60 to 80 percent of cases. Vascular dementia, which occurs after a stroke, is the second most common dementia type. But there are many other conditions that can cause symptoms of dementia, including some that are reversible, such as thyroid problems and vitamin deficiencies.
Dementia is often incorrectly referred to as "senility" or "senile dementia," which reflects the formerly widespread but incorrect belief that serious mental decline is a normal part of aging.
Memory loss and other symptoms of dementia
While symptoms of dementia can vary greatly, at least two of the following core mental functions must be significantly impaired to be considered dementia:
- Memory
- Communication and language
- Ability to focus and pay attention
- Reasoning and judgment
- Visual perception
People with dementia may have problems with short-term memory, keeping track of a purse or wallet, paying bills, planning and preparing meals, remembering appointments or traveling out of the neighborhood.
Many dementias are progressive, meaning symptoms start out slowly and gradually get worse. If you or someone you know is experiencing memory difficulties or other changes in thinking skills, don't ignore them. See a doctor soon to determine the cause. Professional evaluation may detect a treatable condition. And even if symptoms suggest dementia, early diagnosis allows a person to get the maximum benefit from available treatments and provides an opportunity to volunteer for clinical trials or studies. It also provides time to plan for the future.
Causes
Dementia is caused by damage to brain cells. This damage interferes with the ability of brain cells to communicate with each other. When brain cells cannot communicate normally, thinking, behavior and feelings can be affected.
The brain has many distinct regions, each of which is responsible for different functions (for example, memory, judgment and movement). When cells in a particular region are damaged, that region cannot carry out its functions normally.
Understanding Alzheimer's and Dementia outlines the difference between Alzheimer's and dementia, symptoms, stages, risk factors and more.
Different types of dementia are associated with particular types of brain cell damage in particular regions of the brain. For example, in Alzheimer's disease, high levels of certain proteins inside and outside brain cells make it hard for brain cells to stay healthy and to communicate with each other. The brain region called the hippocampus is the center of learning and memory in the brain, and the brain cells in this region are often the first to be damaged. That's why memory loss is often one of the earliest symptoms of Alzheimer's.
While most changes in the brain that cause dementia are permanent and worsen over time, thinking and memory problems caused by the following conditions may improve when the condition is treated or addressed:
- Depression
- Medication side effects
- Excess use of alcohol
- Thyroid problems
- Vitamin deficiencies
Diagnosis of dementia
There is no one test to determine if someone has dementia. Doctors diagnose Alzheimer's and other types of dementia based on a careful medical history, a physical examination, laboratory tests, and the characteristic changes in thinking, day-to-day function and behavior associated with each type. Doctors can determine that a person has dementia with a high level of certainty. But it's harder to determine the exact type of dementia because the symptoms and brain changes of different dementias can overlap. In some cases, a doctor may diagnose "dementia" and not specify a type. If this occurs it may be necessary to see a specialist such as a neurologist or gero-psychologist.
Dementia help and support are available
If you or someone you know has been diagnosed with dementia, you are not alone. The Alzheimer's Association is one of the most trusted resources for information, education, referral and support.
Dementia treatment and care
Treatment of dementia depends on its cause. In the case of most progressive dementias, including Alzheimer's disease, there is no cure and no treatment that slows or stops its progression. But there are drug treatments that may temporarily improve symptoms. The same medications used to treat Alzheimer's are among the drugs sometimes prescribed to help with symptoms of other types of dementias. Non-drug therapies can also alleviate some symptoms of dementia.
Ultimately, the path to effective new treatments for dementia is through increased research funding and increased participation in clinical studies. Right now, volunteers are urgently needed to participate in clinical studies and trials about Alzheimer's and other dementias.
Dementia risk and prevention
Sprint for Discovery
New research shows there are things we can do to reduce the risk of mild cognitive impairment and dementia.
Some risk factors for dementia, such as age and genetics, cannot be changed. But researchers continue to explore the impact of other risk factors on brain health and prevention of dementia. Some of the most active areas of research in risk reduction and prevention include cardiovascular factors, physical fitness and diet.
- Cardiovascular risk factors: Your brain is nourished by one of your body's richest networks of blood vessels. Anything that damages blood vessels anywhere in your body can damage blood vessels in your brain, depriving brain cells of vital food and oxygen. Blood vessel changes in the brain are linked to vascular dementia. They often are present along with changes caused by other types of dementia, including Alzheimer's disease and dementia with Lewy bodies. These changes may interact to cause faster decline or make impairments more severe. You can help protect your brain with some of the same strategies that protect your heart — don't smoke; take steps to keep your blood pressure, cholesterol and blood sugar within recommended limits; and maintain a healthy weight.
- Physical exercise: Regular physical exercise may help lower the risk of some types of dementia. Evidence suggests exercise may directly benefit brain cells by increasing blood and oxygen flow to the brain.
- Diet: What you eat may have its greatest impact on brain health through its effect on heart health. The best current evidence suggests that heart-healthy eating patterns, such as the Mediterranean diet, also may help protect the brain. A Mediterranean diet includes relatively little red meat and emphasizes whole grains, fruits and vegetables, fish and shellfish, and nuts, olive oil and other healthy fats.
-
Back and Neck Pain

Overview
Back pain can range from a mild, dull, annoying ache, to persistent, severe, disabling pain. Pain in your back can restrict mobility and interfere with normal functioning and quality of life. You should always consult your health care provider if you have persistent pain.
Neck pain occurs in the area of the cervical vertebrae in your neck. Because of its location and range of motion, your neck is often left unprotected and subject to injury.
Pain in your back or neck area can be acute. That means it comes on suddenly and intensely. Chronic pain lasts for weeks, months, or even years. The pain can be continuous or intermittent.
What causes back and neck pain?
Even with today's technology, the exact cause of back and neck pain is difficult to determine. In most cases, back and neck pain may have many different causes, including any of the following:
- Overuse, strenuous activity, or improper use, such as repetitive or heavy lifting
- Trauma, injury, or fractures
- Degeneration of vertebrae, often caused by stresses on the muscles and ligaments that support your spine, or the effects of aging
- Infection
- Abnormal growth, such as a tumor or bone spur
- Obesity, which places increased weight on your spine, and pressure on your discs
- Poor muscle tone
- Muscle tension or spasm
- Sprain or strain
- Ligament or muscle tears
- Joint problems, such as arthritis
- Smoking
- Protruding or herniated (slipped) disk and pinched nerve
- Osteoporosis and compression fractures
- Congenital (present at birth) abnormalities of your vertebrae and bones
- Abdominal problems, such as an aortic aneurysm
Where Low Back Pain Begins
Where Neck Pain Begins
What are the symptoms of back and neck pain?
Symptoms associated with back pain may include:
- Dull, burning, or sharp pain in your back. The pain can be confined to a single spot or cover a large area
- Leg numbness or tingling above or below your knee
- Stiffness or achiness that occurs anywhere along your spine (from your neck to your tailbone)
- Sharp, shooting pain that radiates from your low back to your buttocks, down the back of your thigh, and into your calf and toes
- Consistent ache in the middle or lower part of your back, especially after standing or sitting for an extended period
Loss of bladder and bowel control, with weakness in both legs, are symptoms of a serious condition that requires immediate medical attention.
Symptoms associated with neck pain can be:
- Arm numbness or tingling
- Headaches
- Shoulder pain
- Sharp shooting pains or a dull aches in your neck
Pain that occurs suddenly in your back or neck, due to an injury, is considered to be acute pain. Acute pain comes on quickly and may leave sooner than chronic back or neck pain. This type of pain should not last more than 6 weeks.
Pain that may come on quickly or slowly and lingers for weeks, 3 months or greater, is considered to be chronic pain. Chronic pain is less common than acute pain.
How are back and neck pain diagnosed?
If you experience neck or back pain, you should see your health care provider for a medical and physical exam. He or she may also do X-rays of the affected areas, as well as magnetic resonance imaging (MRI). This allows a more complete view. The MRI produces pictures of soft tissues as well, such as ligaments, tendons, and blood vessels. The MRI could lead to a diagnosis of infection, tumor, inflammation, or pressure on your nerve. Sometimes a blood test may help diagnose arthritis, a condition that can cause back and neck pain.
How are back and neck pain treated?
If you experience acute back or neck pain, it may simply improve with some rest. Over-the-counter medicines, such as acetaminophen or ibuprofen, may also help with the discomfort. You should try to move gently during this period, so that you will not become stiff and lose mobility.
If you have chronic pain of your back and neck, you should try several remedies that may be helpful, before seeking surgical options. These include:
- Hot or cold packs (under your health care provider’s instructions)
- Specific exercises to strengthen muscles and ease pain, such as stretching and flexing. Your health care provider can provide and demonstrate these exercises.
- Aerobic exercise may be permitted and can help with your overall fitness and strength
- Certain anti-inflammatory medications or muscle relaxants may be used, with your health care provider’s supervision
- Braces or corsets for extra support
- Injections for pain relief in the area
- Nerve block, which decreases pain signals from the affected nerve
- Acupuncture
How are back and neck pain managed?
Acute back pain usually gets better without special treatment. Using acetaminophen or ibuprofen will decrease pain and help you rest. Surgery and special exercises are generally not used with acute pain.
For severe, disabling, or chronic back and neck pain, rehabilitation programs can be designed to meet your needs. The type of program will depend on the type and severity of your pain, injury, or disease. Active involvement of the patient and family is vital to the success of rehabilitation programs.
The goal of back and neck rehabilitation is to help you manage disabling pain, return to your highest level of functioning and independence possible, while improving your overall quality of life. The focus of rehabilitation is on relieving pain and improving mobility (movement).
To help reach these goals, back and neck rehabilitation programs may include the following:
- Exercise programs to improve range of motion, increase muscle strength, improve flexibility and mobility, and increase endurance
- Help with obtaining assistive devices that promote independence
- Patient and family education and counseling
- Pain management techniques
- Smoking cessation counseling
- Gait (walking) and movement retraining
- Stress management
- Nutritional counseling
- Ergonomic assessments and work-related injury prevention programs
- Vocational counseling
What are the complications of neck and back pain?
- Loss or productivity: Back pain is the most common reason for disability in working adults.
- Nerve damage: If your back pain is from a herniated disc, pressure on the spinal nerves may cause a variety of problems, such as weakness, numbness, or severe shooting pain that travels from the back to the leg.
- Depression: Back or neck pain can disrupt all aspects of a person’s life: work, physical exercise, social activities, and sleep. The anxiety and stress caused by the change in mobility and pain can lead to depression.
- Weight gain: Loss of mobility and inability to exercise can lead to weight gain and the loss of muscle strength.
It is a good idea to see a health care provider if you have numbness or tingling, or if your pain is severe and does not improve with medication and rest. If you have difficulty urinating, weakness, pain, or numbness in your legs, fever, or unintentional weight loss, you should call your health care provider right away.
Can I prevent neck and back pain?
The following may help to prevent back and neck pain:
- Practice correct lifting techniques: avoid heavy lifting; when you do lift something, bend your legs, keep your back straight, and then slowly lift your body and the object.
- Properly use telephones, computers, and other equipment.
- Maintain correct posture while sitting, standing, and sleeping.
- Exercise regularly. Learn specific back-strengthening exercises to keep your back muscles strong. Warm up with stretching exercises before doing back exercises.
- Do exercises that improve your balance.
- Avoid smoking.
- Maintain a healthy weight
- Reduce emotional stress, which may cause muscle tension.
- Make sure you have enough Vitamin D and calcium in your diet.
When should I call my health care provider?
See your health care provider if you have:
- Loss of bladder or bowel control, with weakness in both legs. These symptoms require immediate attention
- Severe back or neck pain that does not decrease with medication and rest
- Pain after an injury or a fall
- Weakness, numbness, or tingling in your legs or arms
- Fever
- Unintentional weight loss
Key points
- Back and neck problems range from minor aches to severe, disabling pain
- Often, the reasons for your pain cannot be identified.
- See a health care provider if you have numbness or tingling, severe pain that does not improve with medication and rest, difficulty urinating, weakness, pain, or numbness in your legs, fever, unintentional weight loss, or pain after a fall.
- Often, back and neck pain will improve over time. Consult with your health care provider if your pain is not decreasing.
- Use prevention strategies to keep yourself healthy and injury-free.
For severe, disabling, or chronic back pain, consider an individualized rehabilitation program.
-
PERIPHERAL NEUROPATHY

Peripheral neuropathy is a general term for any disorder affecting the peripheral nerves. Since peripheral neuropathy can be caused by numerous factors, an investigation into the cause of the neuropathy should be undertaken as soon as the diagnosis of neuropathy is made.
CLINICAL FEATURES
Symptoms Since the peripheral nervous system consists of motor, sensory and autonomic nerves, symptoms can fall into all three of these categories.
- Sensory symptoms include distal dysesthesias, pain and numbness. A characteristic pattern of numbness is one in which the distal portions of the nerves are first affected, the so-called "stocking-glove" pattern. This pattern occurs because nerve fibers are affected according to length of axon, without regard to root or nerve trunk distribution.
- Motor symptoms include weakness, which once again is distal, and typically involves extensor groups rather than flexor groups of muscles.
- Autonomic dysfunction is common and includes orthostasis, impotence in males and gastroparesis. Signs Signs of peripheral neuropathy also include sensory, motor and autonomic components.
- Sensory disturbance is manifest as distal loss of pin, temperature and vibratory perception as well as proprioception. Initial signs are frequently confined to the toes and feet. A positive Romberg sign is frequently present due to proprioceptive loss in the lower extremities.
- Motor signs include distal weakness, primarily in extensor groups, and most prominent in the lower extremities initially. Distal muscles are often atrophic, and one should carefully assess the bulk of the extensor digitorum brevis muscles in the feet and of the intrinsic muscles of the hands. Muscle tone is reduced and often is flaccid.
- Muscle stretch reflexes are frequently lost, and most patients with peripheral neuropathy have absent ankle jerks as one of the first signs of the disorder.
- The most prominent autonomic sign of neuropathy is orthostatic hypotension
CLASSIFICATION
There are many ways to classify peripheral neuropathy. One helpful method is to consider four categories, namely etiology, distribution, pathology and modality.
Etiology
Most peripheral neuropathies fall into three etiologic categories, namely hereditary, toxic/metabolic, and those associated with systemic disease.
Hereditary: This is a large group of disorders in which the onset of symptoms is insidious and progression is indolent over years or decades. Three of these hereditary neuropathies will be discussed:
- Charcot-Marie-Tooth Disease (Hereditary Sensory-Motor Neuropathy [HSMN] I). This is the most common hereditary neuropathy that has an autosomal dominant pattern of inheritance. Phenotypic expression is often variable, such that affected family members of a propositus may have no symptoms and minimal neurologic findings. Characteristic clinical findings include striking atrophy of the calves, resulting in an inverted "champagne-bottle" appearance to the lower extremities. Peripheral nerves are often palpably enlarged. Large fiber sensory loss is present, with a marked reduction in vibratory perception and proprioception. Ankle jerk reflexes are lost. Since this is a demyelinating polyneuropathy, nerve conduction velocity measurements are characteristically slow, at approximately 50% of normal values.
- Dejerine-Sottas Disease (HSMN III). This is a rare pediatric disorder with autosomal recessive inheritance that causes severe weakness and numbness, markedly enlarged peripheral nerves with "onion-bulb" formation and markedly slowed conduction velocities.
- Refsum's Disease (HSMN IV). This autosomal recessive disorder is caused by an enzymatic defect that results in accumulation of phytanic acid. The clinical triad includes peripheral neuropathy, retinitis pigmentosa and dry, scaly skin. Treatment includes dietary restriction of phytanic acid and plasmapheresis.
Toxic/Metabolic: Numerous drugs and toxins can cause peripheral neuropathy. A partial list follows:
- Drugs: amiodarone, cis-platinum, dapsone, INH, phenytoin, pyridoxine, vincristine, nitrofurantoin, ddI, ddC.
- Toxins: heavy metals including mercury, arsenic, lead, zinc and thallium; alcohol; and the organophosphates.
Neuropathy Associated with Systemic Diseases:
- Numerous systemic diseases are associated with neuropathy. Among the most common systemic disorders are: uremia; porphyria; vitamin B12 deficiency; amyloidosis; hypothyroidism; lymphoma, including Hodgkins' disease; multiple myeloma; cryoglobulinemia; vasculitis, including systemic lupus erythematosus (SLE), rheumatoid arthritis and polyarteritisnodosa; sarcoidosis; and benign monoclonal gammopathy, including IgG, IgA and IgM.
- A purely sensory neuropathy can be seen with several carcinomas, especially oat cell carcinoma of the lung.
- Four systemic infections have a high incidence of neuropathy, including leprosy, syphilis, HIV and diphtheria.
- Diabetes mellitus is perhaps the most common cause of neuropathy in India. Both symmetric and asymmetric diabetic neuropathies can occur, as follows:
- Symmetric polyneuropathies: These are the most common and include a sensory/motor polyneuropathy and an autonomic neuropathy.
- Asymmetric neuropathies are less common. Mononeuropathy multiplex results in simultaneous dysfunction of several peripheral nerves, and is due to ischemic infarction of the vasa nervorum. Cranial neuropathies, truncal radiculopathies and diabetic amyotrophy (ischemic infarction of the lumbosacral plexus) are other forms of asymmetric neuropathies. Entrapment neuropathies, including carpal tunnel syndrome, are also commonly seen in diabetics. Distribution Nerve damage in peripheral neuropathy may be symmetrical generalized, multifocal or focal.
- Symmetrical generalized polyneuropathies produce signs and symptoms in a distal-to-proximal gradient, the so-called "stocking-glove" pattern. The reason for this is that the "offending agent" causing the neuropathy affects protein synthesis in the cell body of the peripheral nerve. Hence, neuronal dysfunction will first occur in the distal portions of the longest axons, and thus produce symptoms of weakness and numbness in the most distal portions of the extremities, i.e. the feet and hands.
- Multifocal Neuropathies (Mononeuropathy Multiplex): Patients with these forms of neuropathy develop more-or-less simultaneous dysfunction of several peripheral nerves. The underlying pathologic mechanism is felt to be ischemic infarction of the vasa nervorum due to vasculitis, as can occur with SLE, rheumatoid arthritis, polyarteritisnodosa and diabetes mellitus. These neuropathies are frequently painful and cause profound weakness. Prognosis for recovery is good, assuming that the underlying disease process leading to nerve infarction can be suppressed.
- Focal Neuropathies (Mononeuropathies): Traumatic injuries and entrapment of peripheral nerves at the usual sites of compression are the most common causes of focal mononeuropathy.
The most frequently seen entrapment neuropathies include:
- Compression of the median nerve across the wrist (carpal tunnel syndrome)
- Compression of the ulnar nerve across the elbow (tardy ulnar palsy)
- Compression of the radial nerve at the spiral groove (Saturday night palsy)
- Compression of the peroneal nerve at the fibular head (peroneal nerve palsy)
- Compression of the distal branches of the tibial nerve at the ankle (tarsal tunnel syndrome)
Pathology
There are three major pathologic mechanisms causing peripheral neuropathy: distal axonopathy, myelinopathy, and neuronopathy.
- Distal Axonopathy: In this form of neuropathy, a metabolic abnormality causes failure of protein synthesis and axonal transport, resulting in degeneration of distal regions of axons. For this reason, axonal neuropathies characteristically produce a "stocking-glove" distribution of numbness and weakness. Small-diameter axons are most susceptible to metabolic injury because of their small neuronal size and lack of "reserve". Hence, initial symptoms of an axonal neuropathy typically include autonomic dysfunction and small-fiber sensory modalities, including loss of pain and temperature perception, since these modalities are subserved by small, unmyelinated or thinly myelinated axons.
- Myelinopathy: An immune-mediated attack on peripheral nervous system myelin is the characteristic pathologic change in this group of neuropathies. Guillain-Barre syndrome (GBS) and chronic inflammatory demyelinating polyneuropathy (CIDP) are the two most common forms of demyelinating polyneuropathy. GBS is a monophasic, immune-mediated demyelinating neuropathy that frequently follows a viral infection and causes an acute and frequently severe progression of weakness and numbness over several weeks. CIDP is a chronic demyelinating polyneuropathy that can have a slowly progressive or a relapsing course. In both of these neuropathies antibodies have been found that cross-react with peripheral nerve myelin. Elevated CSF protein and slowed nerve conduction velocities are characteristic of the demyelinating neuropathies. In general, demyelinating neuropathies affect large-diameter, myelinated axons at the start of the illness, and hence produce significant motor weakness and large-fiber sensory loss, including loss of vibratory perception and proprioception. In diphtheritic neuropathy, the bacterium produces a toxin that inhibits Schwann cell synthesis of myelin constituents, producing severe weakness and large-fiber sensory loss.
- Neuronopathy: Selective involvement of the cell bodies of motor, sensory and autonomic nerves is the hallmark of this group of neuropathies.
- Somatic motor neuronopathies result from isolated involvement of the anterior horn cells. Amyotrophic lateral sclerosis and the spinal muscular atrophies are two examples of somatic motor neuronopathies.
- Somatic sensory neuronopathies result from disruption of the metabolism of sensory nerve cell bodies, followed by degeneration of their processes. Special permeability of the blood vessels in the dorsal root and Gasserian ganglia make these neurons particularly vulnerable to certain toxins. Two common examples of somatic sensory neuronopathies include the paraneoplastic subacute sensory neuropathy seen with oat-cell carcinoma of the lung, and the sensory neuronopathy associated with Sjogren's syndrome.
- Autonomic Neuronopathy: This unusual group of neuropathies results from isolated involvement of post-ganglionic autonomic neurons and causes idiopathic orthostatic hypotension. Modality Peripheral neuropathies can be sub-classified based on their involvement of motor, sensory or autonomic neurons
- Modality-Specific Neuropathies: The somatic motor, somatic sensory and autonomic neuronopathies described above are examples of modality-specific neuropathies. The pathologic lesion in this group of neuropathies is confined to the cell bodies.
- Mixed-Modality Neuropathies: The majority of peripheral neuropathies is not modality-specific, and includes various combinations of motor, sensory and autonomic dysfunction. The reason for this finding is that most peripheral nerves include a mixture of motor, sensory and autonomic axons. Hence, axonal neuropathies typically present with mixed symptomatology. Likewise, since most axons are myelinated to a greater or lesser extent, demyelinating neuropathies also produce a mixture of motor, sensory and autonomic symptoms.
The mnemonic DANG THERAPIST is helpful in recalling the more common causes of peripheral neuropathy: Diabetes Mellitus Alcohol Nutritional (B12 deficiency) Guillain-Barre Syndrome Toxins (Pb, As, Zn, Hg) Hematologic (paraproteins) Endocrine (hypothyroid) Rheumatologic (SLE, rheumatoid arthritis, vasculitis) Amyloid Porphyria Infectious (syphilis, HIV) Sarcoid Tumor (paraneoplastic neuropathy)
LABORATORY INVESTIGATION
Laboratory studies play an important role in diagnosing and categorizing the peripheral neuropathies. Electrodiagnostic studies are helpful in quantitating the neuropathy, while blood and urine studies are helpful in identifying an etiology.
Electrodiagnostic Studies
- Nerve Conduction Study: The recording and measurement of the compound nerve and muscle action potential elicited in response to a single supramaximal electrical stimulus, to measure the terminal latency, amplitude and duration of the evoked potential, as well as the conduction velocity. Nerve conduction studies are helpful in documenting that a neuropathy exists, quantitating the severity, and noting the distribution of the neuropathy, i.e. whether it is distal, proximal or diffuse. In addition, nerve conduction studies can provide information on the modality involved, i.e. motor versus sensory, and can also give clues as to the underlying pathology, whether axonal or demyelinating. Demyelinating neuropathies (neuropathies due to loss or destruction of myelin) result in slowed conduction velocities and prolonged distal latencies, because conduction velocity is proportional to the velocity of the largest-diameter myelinated fibers. Dispersion of evoked compound action potentials (CAP) can also be seen in demyelinating neuropathies, because all of the action potentials elicited in response to a single electrical stimulus will not reach the recording potential at the same time. Severe demyelinating neuropathies can also produce conduction block, which is a major decrease in amplitude of the muscle CAP upon proximal stimulation of its nerve as compared to distal stimulation. Axonal neuropathies (neuropathies due to loss of axons or their cell bodies) generally result in a reduced amplitude of the compound motor or sensory nerve action potentials.
- Electromyography (EMG): The recording and study of insertional, spontaneous, and voluntary electrical activity of muscle. This test allows one to physiologically evaluate the motor unit, including the anterior horn cell, peripheral nerve, and muscle. EMG is helpful when evaluating patients with weakness, in that it can help one determine whether weakness is due to anterior horn cell disease, nerve root compression, peripheral neuropathy, or an intrinsic disease of muscle itself (myopathy). EMG can differentiate acute denervation from chronic denervation, and may thus give an indication as to the time course of the lesion causing the neuropathy.
- Acute Denervation: Fibrillations and positive waves are present indicating spontaneous discharge of individual muscle fibers.
- Chronic Denervation: Voluntary motor unit potentials are of large amplitude and long duration, and are frequently polyphasic, because the motor units are enlarged as a result of re-innervation of adjacent previously denervated muscle fibers. Recruitment of additional motor units in response to increasing the force of muscular contraction is reduced for the same reason.
- Demyelinating Neuropathy: A decreased recruitment pattern is seen, since demyelination interferes with conduction of individual action potentials along the course of a peripheral nerve. Because denervation and reinnervation of muscle fibers are not features of demyelinating neuropathies, the configuration of the voluntary motor unit potentials is usually normal, and fibrillation potentials are not seen.
Nerve Biopsy
There are few indications for nerve biopsy when evaluating peripheral neuropathy. In general, a nerve biopsy is performed to evaluate asymmetric, multi-focal neuropathies. The sural nerve is frequently biopsied, since this is a purely sensory nerve that is easily obtained. In the upper extremity, the superficial radial nerve may be biopsied if necessary. The nerve specimen is typically evaluated by means of light and electron microscopy. Semi-thin plastic embedded sections, stained with toluidine blue, are helpful for evaluating the myelin sheaths. Teased nerve fiber preparations are also helpful to look for demyelination and remyelination.
Sural nerve biopsies are particularly helpful when evaluating patients with a clinical picture of mononeuropathy multiplex, the basis of which is still unclear after other laboratory investigations are complete. Vasculitis, amyloidosis, leprosy and sarcoidosis can be accurately diagnosed by means of nerve biopsy. Performing a nerve biopsy routinely in the evaluation of symmetric, distal polyneuropathies is usually fruitless, in that the pathologic diagnosis most often reveals "chronic neuropathy with mixed axonal-demyelinating features", a non-specific finding of little clinical benefit.
Blood Studies Routine blood studies should be obtained in all patients with peripheral neuropathy in order to screen for reversible causes.
The following blood tests are recommended:
- Complete blood count
- Chemistry profile
- Sedimentation rate
- Thyroid studies
- Vitamin B12 level
- ANA, rheumatoid factor
- Serum protein electrophoresis, serum immuno-electrophoresis
- RPR and HIV (if the clinical situation warrants)
Urine Studies
The following studies are recommended to screen for reversible causes of neuropathy:
- Heavy metal screen (Hg, Pb, Zn, As)
- Urine protein electrophoresis, urine immuno-electrophoresis
- Watson-Schwartz test (qualitative test for porphobilinogen)
Chest x-ray, helpful to screen for asymptomatic lung cancer that can sometimes cause a purely sensory neuropathy.
TREATMENT
Neuropathy Associated With Systemic Illness
Treatment of the systemic illness frequently results in improvement in neuropathic symptoms. Since nerves regenerate slowly, at a rate of about one mm per day, recovery is often prolonged and may take months to years.
Immune-mediated Neuropathies
The immune-medicated neuropathies include those associated with vasculitis (SLE, rheumatoid arthritis or polyarteritisnodosa), and the immune-mediated demyelinating neuropathies (Guillain-Barre syndrome and CIDP).
- Corticosteroids: By virtue of their immunosuppressive effects, corticosteroids have been found to be effective in treating the vasculitic neuropathies as well as CIDP. Corticosteroids may be given daily or on an every-other-day regimen, depending on the severity and tempo of the disease. The typical initial dose of corticosteroids for the treatment of these neuropathies is 1 mg/kg/day of prednisone (or 2 mg/kg every-other-day). Corticosteroids have never been proven to be effective in treating Guillain-Barre syndrome, and hence are not recommended for this disorder.
- Immunosuppressives: Azathioprine, cyclophosphamide, cyclosporine, mycophenolate and methotrexate are all used in the treatment of autoimmune diseases. Each of these medications has potential serious toxicity. Azathioprine is frequently used, in combination with steroids, to treat autoimmune neuropathies because of its steroid-sparing effect. Concurrent use of these two medications allows corticosteroids to be tapered more quickly and more completely once the neuropathy is brought under control. The usual dosage of azathioprine is 2-3 mg/kg/day given in divided doses. This medication has a delayed beneficial effect and several months are required before an effect may be seen. The erythrocyte mean cell volume (MCV) provides an index of therapeutic effect: a slight elevation in MCV suggests that the dose of azathioprine is appropriate. Azathioprine is metabolized by xanthine oxidase, and medications that block this enzyme, such as allopurinol, should be avoided since concurrent use can cause azathioprine toxicity.
- Plasmapheresis: In this procedure, blood is removed from the patient, plasma is separated from blood cells and discarded, and blood cells are resuspended in colloid solution and reinfused. Plasmapheresis is effective in treating patients with immune-mediated neuropathies such as those caused by cryoglobulins, SLE, rheumatoid arthritis or polyarteritisnodosa. In addition, individuals with GBS and a large subset of patients with CIDP benefit from this procedure. The effects of plasma exchange can be summarized as "fast, temporary, and expensive". This procedure does not, by itself, induce permanent remission, and the 10 ideal application is therefore in acute, self-limited disorders such as GBS. Plasma exchange may also have application in chronic diseases, such as CIDP, where rapid therapeutic effects may occasionally be required.
- Intravenous Immunoglobulin (IVIg):IVIg is pooled, human IgG in a form that is safe for intravenous administration. How IVIg affects immunologic function is unknown, but three putative mechanisms have been postulated:
- Administration of IVIg floods the recipient with an enormously diverse array of antibody molecules, some of which are anti-idiotypic antibodies which may neutralize auto-antibodies in the patient, thereby increasing their clearance and perhaps downregulating their production.
- IVIg inhibits the binding of activated complement to target cells, thus reducing complement-mediated damage to cell membranes.
- IVIg infusion is a potent stimulus that down-regulates immunologic production. To date, IVIg has been found to be as effective as plasma exchange in treating many immunologic disorders, including Guillain-Barre syndrome and CIDP. IVIg is also reported to be beneficial in treating the polyneuropathy associated with IgG or IgM paraproteins. Side effects of IVIg include fever, myalgia, headache, rash, and occasionally aseptic meningitis and renal failure. The cost of IVIg is equivalent to that of plasma exchange.
Symptomatic Treatment
Numerous symptomatic treatments for the pain of peripheral neuropathy are available, and all have their relative risks and benefits.
- Tricyclic Compounds: Drugs in this category include amitriptyline, nortriptyline, desiprimine, imiprimine and duloxetine. These drugs inhibit the re-uptake of the catecholamine neurotransmitters epinephrine and norepinephrine as well as serotonin, and thus may enhance central pathways that suppress pain transmission. The tricyclic compounds are quite useful for treatment of the burning, dysesthetic pains seen with peripheral neuropathies. Most of these drugs are sedating and, when given at bedtime, promote sleep. Effective dosages of these drugs for treating chronic neuropathic pain are typically lower than the dosages used for treating depression. We recommend starting with a low single dose at bedtime and slowly increasing the dose over several weeks. Patients should be informed that it may take several weeks before full therapeutic effects are realized.
- Anticonvulsants: Drugs in this category include carbamazepine, phenytoin, gabapentin and lamotrigine. These drugs stabilize neuronal membranes and may thus prevent neuronal “shortcircuits” that lead to neuropathic pain. The anticonvulsant drugs are quite useful in treating the lancinating pains frequently seen with trigeminal neuralgia and in some other peripheral neuropathies. Effective dosages for treating neuropathic pain are similar to the dosages used for treating seizures. Blood levels of these drugs may be monitored and dosages adjusted as needed. Lamotrigine, a new anti-seizure drug effective for primary generalized seizures, can cause a severe and fatal cutaneous hypersensitivity reaction if the starting dosage is high, and therefore must be started at a very low dose with a very gradual dosage escalation.
- Topicals: Capsaicin, a drug that impedes pain transmission by depleting substance P from sensory nerve fibers, has been found effective in treating refractory neuralgia in several studies. The cream must be applied several times daily to be effective, and patients frequently experience severe burning following each application for one or two weeks following initiation of treatment. Transdermal lidocaine (Lidoderm), a local anesthetic, also appears to be effective for some patients with neuropathic pain syndromes. This drug is available as an adhesive patch that may be cut to size and replaced every 12 hours. Surgery Surgical release of tendons, scar tissue and bony ridges is beneficial in treating many forms of entrapment neuropathy. Nerve transposition may play a role as well in certain clinical circumstances.
-
Other Neuromuscular Disorders
- Myasthenia Gravis – a chronic autoimmune disorder, this disease blocks the signals from the nerves to the muscles and makes the muscles unable to move. A key indication of the disease is muscle weakness that increases during periods of activity and improves after periods of rest. The good news is that in majority, if this disease is treated early patient improves after initiation of therapy.
- Myopathy – a disorder of the muscles, myopathy is characterized by muscle weakness that is usually the most severe in the upper arms and thighs.
- Amyotrophic Lateral Sclerosis – also known as ALS or Lou Gehrig’s disease, this is a progressive disease affecting motor neurons and causes deterioration of the body’s muscle function. There is no known cure for ALS.
-
Demyelinating Disorders of brain
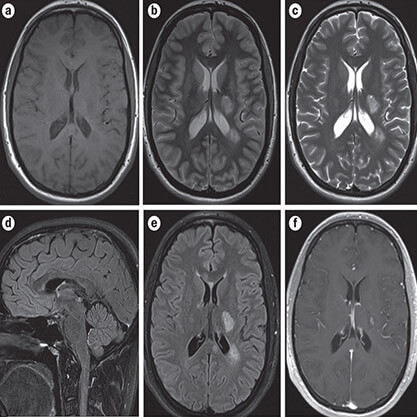
Also known as: demyelination, demyelinating diseases of the brain, ADEM (acute disseminated encephalomyelitis), MS (multiple sclerosis), Optic neuritis, NMO (Neuromyelitisoptica), ATM (acute transverse myelitis).
What is demyelinating disease?
The myelin sheath is a protective fatty material that wraps, protects and insulates the nerve fibers of the brain, spinal cord and peripheral nerves. It enables brain signals to travel quickly along nerves to the rest of the body. Any disease that causes damage to the myelin sheath that slows or stops nerve signals is called a demyelinating disease. There are a number of demyelinating diseases in childhood, of which Pediatric Multiple sclerosis (MS) is an uncommon one.
What causes demyelinating disease?
Causes are multifactorial and include genetic, postinfectious, post-immunization, and autoimmune (the body produces proteins which damage its own tissue).
What are the symptoms of demyelinating disease?
There are many common clinical, radiological and laboratory features and a wide variation in the way each particular disease presents, develops, which and how many nerves are involved, and whether the process fluctuates (gets better than worse again) or not. Symptoms of demyelinating disease can include muscle weakness, muscle spasms, loss of coordination, pain, vision loss, changes in bladder and bowel function and other problems.
What are demyelinating disease care options?
No cure exists for demyelinating diseases; early recognition, supportive care and early treatment with medications may help minimize and manage symptoms. Rehabilitation therapies are of particular importance.
-
Brain Infections
Also known as: inflammatory brain disease, spinal inflammatory disorders, abscess, meningitis, encephalitis.
What are brain infections?
The brain and its coverings (meninges) can become infected by a wide variety of infections which include bacteria, viruses and uncommonly parasites and fungi. Depending on the part of the brain involved, different names are given to the diseases. Meningitis, is the inflammation of the brain’s surrounding tissues (meninges) - Encephalitis is an inflammation of the brain itself- Brain abscess is the localized collection of inflammation cells and fluids.
What causes brain infections?
Brain infections occur from an infection with bacteria, viruses, fungi or parasites.
Infants may acquire a brain infection from their mother prior to or during birth. Children at increased risk for developing a brain infections include those who have a infection of the coverings of the brain (meningitis); a congenital heart defect; chronic ear and sinus infection; teeth and jaw infections; the presence of foreign material involving the brain (like cerebrospinal shunts); diabetes and children who have congenital or acquired difficulty in fighting infections (immune problems).
What are the symptoms of brain infections?
In babies and young infants, symptoms include; fever, a full/bulging fontanelle drowsiness and/or irritability, a high pitched cry, difficulty feeding, vomiting and seizures.
Older children may present with gradual or sudden; fever, vomiting, headache, seizures, stiff limbs, behavior and/personality changes and difficulty talking and walking.
What are brain infection care options?
Depending on a number of factors, the goal of management is to diagnose and treat the problem early. Hospitalization with antibiotics, (where appropriate), with other medications as needed, depending on complications present. Physical, occupational and speech therapy may be required subsequently to assist the child to reach his/her full potential.
-
Electroencephalogram (EEG)
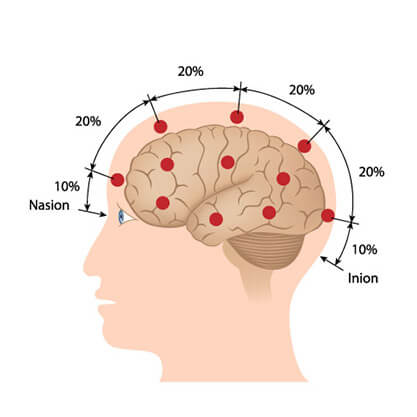
Electroencephalography (EEG) is the measurement of electrical activity produced by the brain as recorded from electrodes placed on the scalp.
An EEG is used to help diagnose the presence and type of seizure disorders, confusion, head injuries, brain tumors, infections, degenerative diseases, and metabolic disturbances that affect the brain. It is also used to evaluate sleep disorders and to investigate periods of unconsciousness.
Preparation:
Please wash your hair the night before the test. No oils, sprays, or lotion should be used on your hair.Please avoid all foods/drinks containing caffeine for 8 hours before the test.
It may be necessary to sleep during the test, so you may be asked to reduce your sleep time the night before.
Procedure:
This procedure is performed by an EEG technician and typically lasts 20-40 minutes.
You may be positioned on your back, on a table, or in a reclining chair.
The technician will apply between 16 and 25 flat metal discs (electrodes) in different positions on your scalp.The discs are held in place with a sticky paste. The electrodes are connected by wires to an amplifier and the recording machine which converts the electrical signals into a series of wavy lines which are drawn onto a moving piece of graph paper.This procedure is painless.
Video-EEG Monitoring
A video EEG (electroencephalograph) records what you are doing or experiencing on video tape while an EEG test records your brainwaves. The purpose is to be able to see what is happening when you have a seizure or event and compare the picture to what the EEG records at the same time. Sounds that occur during the testing are also recorded - this can pick up if a person talks or makes sounds during an event. By doing this, doctors reading the EEG can tell if the seizure or event was related to the electrical activity in the brain. If so, we'd call this an epilepsy seizure. The "gold standard" in the diagnosis of nonepileptic seizures (NESs) is a recording of a typical event during video-EEG monitoring.
Video EEG is most helpful to determine if seizures with unusual features are actually epilepsy, to identify the type of seizures, and to pinpoint the region of the brain where seizures begin. Locating the region precisely is essential if epilepsy surgery is being considered.
Other names for video EEG tests include: EEG telemetry, EEG monitoring, or video EEG monitoring. Usually these terms mean the same thing.
-
NCS( NERVE CONDUCTION STUDY)

Nerve Conduction Study (NCS)
A nerve conduction study (NCS) is a test commonly used to evaluate the function, especially the ability of electrical conduction, of the motor and sensory nerves of the human body.
Nerve conduction studies are mainly used for the evaluation of paresthesias (numbness, tingling, burning) and/or weakness of the arms and legs. It can be used to diagnose disorders of the peripheral nerves and muscles.
Preparation:
No special preparation is required before the test.
Procedure:
This procedure is performed by an NCV technician and typically lasts 15-30 minutes.
-
EMG (ELECTROMYOGRAM)
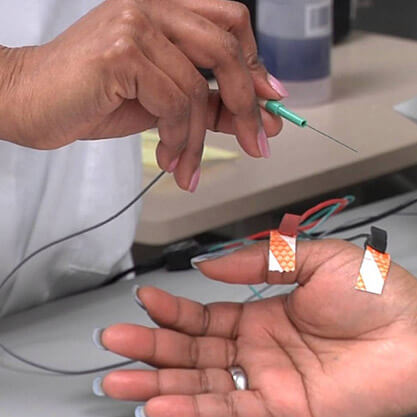
An EMG, used in conjunction with a neurological examination, and nerve conduction study helps establish a diagnosis and the extent of a problem by measuring the electrical activity of a muscle in response to stimulation.
An EMG is done by inserting electrodes in fine needles into the muscles being tested, and by placing electrodes on the skin over peripheral nerves.
The presence, size, and shape of the wave form produced on the oscilloscope (the action potential) provide information about the ability of the muscle to respond to nervous stimulation.
Each muscle fiber that contracts will produce an action potential and the size of the muscle fiber affects the rate (how frequently an action potential occurs) and size (amplitude) of the action potential(s).
An EMG may be used to evaluate a variety of problems, including the following:
- Nerve damage from compression by a disk in the neck or the back
- Nerve compression from carpal tunnel syndrome
- Neuromuscular diseases such as amyotrophic lateral sclerosis (ALS), poliomyelitis, myasthenia gravis and muscular dystrophy
- Peripheral neuropathy caused by such conditions as diabetes, pernicious anemia and heavy metal toxicity
- In many instances, an EMG can provide critical diagnostic information that can not be obtained in any other way.
Preparation:
No special preparation is required before the test.
Procedure:
This procedure is performed by an EMG technician and typically lasts 15-30 minutes.
-
VEP (VISUAL EVOKED POTENTIAL)

A visual evoked potential is an evoked potential caused by a visual stimulus, such as an alternating checkerboard pattern on a computer screen. Responses are recorded from electrodes that are placed on the back of your head and are observed as a reading on an electroencephalogram (EEG). These responses usually originate from the occipital cortex, the area of the brain involved in receiving and interpreting visual signals.
A doctor may recommend that you go for a VEP test when you are experiencing changes in your vision that can be due to problems along the pathways of certain nerves. Some of these symptoms may include:
- Loss of vision (this can be painful or non-painful)
- Double vision
- Blurred vision
- Flashing lights
- Alterations in colour vision
- Weakness of the eyes, arms or legs
In general terms, the test is useful for detecting optic nerve problems. This nerve helps transfer signals to allow us to see, so testing the nerve allows the doctor to see how your visual system responds to light. The test is also useful because it can be used to check vision in children and adults who are unable to read eye charts.
The VEP measures the time that it takes for a visual stimulus to travel from the eye to the occipital cortex. It can give the doctor an idea of whether the nerve pathways are abnormal in any way. For example, in multiple sclerosis, the insulating layer around nerve cells in the brain and spinal cord (known as the myelin sheath) can be affected. This means that it takes a longer time for electrical signals to be conducted from the eyes, resulting in an abnormal VEP. A normal VEP can be fairly sensitive in excluding a lesion of the optic nerve, along its pathways in the anterior part of the brain.
Preparation:
You will be given instructions on how to prepare for the test. This will depend on where you are going to get the test done. Some things that you may need to do include:Washing your hair the night before, but avoiding hair chemicals, oils and lotions.Making sure you get plenty of sleep the night before.If you wear glasses, make sure you bring these along with you to the test.
You are usually able to eat a normal meal and take your usual medications prior to the test. However any medications that may make you drowsy should be avoided.
Arrive on time and try to relax before the test.
On the day of the test, you should also let the technician know if you have any eye conditions such as cataracts or glaucoma as this can affect the test and should be noted in your records by the doctor.
Procedure:
This procedure is performed by an EEG technician and typically lasts 30-45 minutes. The procedure is very safe and non-invasive.Firstly, some wires will be glued to the top of your head to detect the brain waves.
A technician will give you further instructions on what to do during the test. Normally, each eye will be tested separately.
It is very important that you co-operate with the technician who conducts the test and be able to fix your vision in a certain spot. You will be asked to look at a screen similar to a television screen, with various visual patterns.
Readings will be recorded through the wires on top of your head.There are no side effects from this procedure. It is a painless procedure and apart from possible minor skin irritation from the electrodes, there are often no complications. You should be able to drive home safely if you are feeling well after the procedure.
-
Brainstem Auditory Evoked Response(BAER)

A brainstem auditory evoked response (BAER) test measures how your brain processes the sounds you hear. The BAER test records your brainwaves in response to clicks or other audio tones that are played for you. The test is also called a brainstem auditory evoked potentials (BAEP) or auditory brainstem response (ABR) test.
A BAER test can help to diagnose hearing loss and nervous system disorders, especially in newborns, young children, and others who may not be able to participate in a standard hearing test.
BAER tests are often administered to canines and are the only scientifically reliable way to test a dog’s ability to hear with one or both ears.
BAER tests are quick and easy, and have virtually no risks or complications. You do not need to prepare for the test in advance, though you may be asked to wash your hair the night before to remove oils that might keep the testing equipment from sticking to your scalp.
You will simply lie back in a reclining chair or on a bed and keep still while the doctor places small electrodes (sticky patches with wires attached) on your scalp and earlobes. The electrodes are connected to a machine that records your brain activity. If your infant or child is being tested and cannot remain still, the doctor may give them a sedative medication.
The doctor will then give you a set of earphones. You should hear a series of clicks or tones played through the earphones, but you do not need to do anything in response to the sounds. The electrodes placed on your scalp and earlobes will record how your brain reacts to the noises you hear. It will show if you are hearing the sounds properly and if they are being conducted from your ears to your brain.
A printout of your test results should show spikes in your brain activity each time you heard one of the clicking sounds or other tones. If your results show flat lines when one of the tones or clicking sounds was played, it may indicate that you have hearing loss.
Abnormal test results can also indicate that you have sustained damage to your brain or nervous system. This could be caused by:
- multiple sclerosis (an autoimmune disease that causes damage to the protective coverings of your nerve cells)
- central pontine myelinolysis (another condition that damages the myelin sheath covering your nerve cells)
- acoustic neuroma (a tumor growing on the nerve that connects your ear to your brain)
- a stroke
- a brain injury
- a brain tumor
- a speech disorder
Additional tests will probably be required to determine the cause if your test results are abnormal,. Once the underlying cause has been identified, your doctor will discuss your treatment options with you.
-
Somatosensory Evoked Potential (SSEP)

Somatosensory Evoked Potential (SSEP) is a test showing the electrical signals of sensation going from the body to the brain. The signals show whether the nerves that connect to the spinal cord are able to send and receive sensory information like pain, temperature, and touch. When ordering electrical tests to diagnose spine problems, SSEP is combined with an electromyogram (EMG), a test of how well the nerve roots leaving the spine are working. An SSEP indicates whether the spinal cord or nerves are being pinched. It is helpful in determining how much the nerve is being damaged and if there is a bone spur, herniated disc, or other source of pressure on the spinal cord or nerve roots. EMG is used to show if a nerve is being irritated or pinched as it leaves the spine on its way down the arm or leg. During spine surgery, the EMG is used to monitor nerve output to the muscles in procedures where screws are placed in the middle or lower part of the spine. SSEP is used to double check whether the sensory part of the nerve is working correctly. Either an electrode is placed over the skin or a needle is inserted into the nerve or sensory center of the brain. Measurements of how long it takes an electrical signal to travel through the nerve pathway are recorded. The function of the nerve is determined by the speed of these electrical signals. When the nerve pathway is pinched, the signals are slower than expected.
-
AUTONOMIC TESTING (FIRST TIME ONLY CENTRE IN JHARKHAND)

Autonomic Testing
Autonomic tests measure how the systems in the body that are controlled by the autonomic nerves respond to stimulation. The data collected during testing will indicate if the autonomic nervous system is functioning as it should, or if nerve damage has occurred.
What is it?
The nervous system has three parts: motor, sensory and autonomic. The autonomic system manages all internal functions such as blood pressure, blood flow, and sweating. Autonomic tests are conducted to see if the autonomic nervous system is functioning normally.
Why do it?
Autonomic testing can help determine if a patient is suffering from certain diseases that attack the autonomic nervous system, or as a way to diagnose an illness, or source of pain.
How is it performed?
To see if a disease is affecting the autonomic nervous system, several tests are done to monitor blood pressure, blood flow, heart rate, skin temperature, and sweating. By measuring these functions, it is possible to discover whether or not the autonomic nervous system is functioning normally.
Tests to measure blood pressure and heart rate include the tilt table test, a deep breathing test and the Valsalva maneuver. The tilt table test requires that the patient lie on a table that is then raised. The deep breathing test requires the patient to take deep breaths for a minute. The Valsalva maneuver requires that the patient blow into a tube to increase pressure in the chest. While these simple tests are performed, blood pressure and heart rate are monitored.
The Quantitative Sudomotor Axon Reflex Test (QSART) described separately, is another autonomic test performed to measure sweating and skin temperature.
-
CSF STUDY:
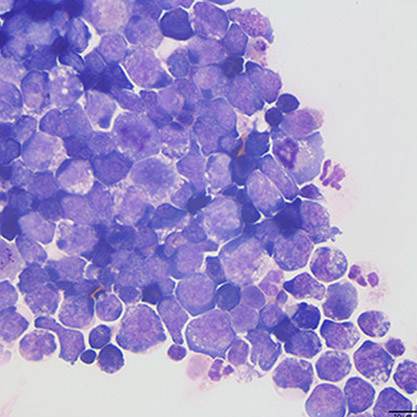
Cerebrospinal fluid (CSF) collection is a test to look at the fluid that surrounds the brain and spinal cord. Cerebrospinal fluid acts as a cushion, protecting the brain and spine from injury. The fluid is normally clear. The test is also used to measure pressure in the spinal fluid.This test is done to measure pressures within the cerebrospinal fluid and to collect a sample of the fluid for further testing. CSF analysis can be used to diagnose certain neurologic disorders, particularly infections (such as meningitis) and brain or spinal cord damage.
-
BOTOX (BOTULINUM TOXIN) THERAPY

Botulinum toxin injection (Botox) is a neuromuscular blocking agent used in the treatment of excessive muscle activity. Patients who are diagnosed with movement disorders such as dystonia, hemifacial spasm and blepharospasm are treated with Botox injections. These injections are effective with lower side effects in patients who suffer from drooling in Parkinson’s disease.
Botulinum toxin is effective in treating a variety of neurological conditions including:
- Cervical dystonia / spasmodic torticollis
- Hemifacial spasm - twitching of the muscles on one side of the face
- Blepharospasm - Uncontrolled blinking
- Spasticity following stroke
- Hyperhidrosis (excessive sweating)
- Prophylaxis of chronic migraine
- Headache and other painful conditions
- The goal of the therapy is to reduce muscle spasm and pain, and restore more useful function. A very small dose of botulinum toxin is injected into a muscle to block some of the messages that are sent from the nerves to the muscles, reducing spasms. Physical or occupational therapy occasionally helps restore normal muscle function.
When a patient comes to our clinic for consultation, we conduct thorough evaluation to determine if Botox therapy is an appropriate treatment for him. Botox therapy is an outpatient treatment and we take extra care when treating our patients with this method. Patients begin to experience the effects of the injection in one or two weeks.
-
Nerve and Muscle Biopsy
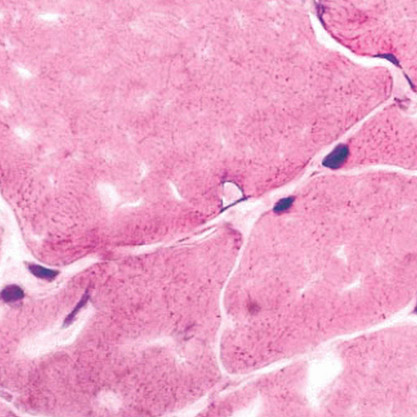
There are multitude of neuromuscular diseases that are exceptionally difficult to diagnose. In some cases, even extensive clinical examination and laboratory workups fail to reveal a diagnosis. In these cases, a nerve and or a muscle biopsy might be required to secure a diagnosis. Once a definitive diagnosis is obtained, the appropriate prognosis and treatments may be provided.
Essentially any nerve or muscle in the body can used for biopsy. The majority of biopsies sample muscles and nerves that are surgically-accessible with a local anesthetic with a minimum of effort. These procedures are almost invariably tolerated quite easily by awake patients.
Common muscles subjected to biopsy are the quadriceps, deltoid, biceps, gastrocnemius, and gracilis muscles.
Common nerves subjected to biopsy are the superficial peroneal, sural, superficial radial sensory, and gracilis.
The gracilis nerve is a motor nerve that supplies the gracilis muscle in the thigh. As a motor nerve, it is an extremely useful nerve used in the diagnosis of motor neuron diseases such as amyotrophic lateral sclerosis (ALS).
-
PHYSICAL MEDICINE & REHABILITATION

Physical medicine and rehabilitation (PM&R), also known as physiatry or rehabilitation medicine, aims to enhance and restore functional ability and quality of life to those with physical impairments or disabilities affecting the brain, spinal cord, nerves, bones, joints, ligaments, muscles, and tendons. Unlike other medical specialties that focus on a medical “cure,” the goals of the physiotherapist/physiatrist are to maximize patients’ independence in activities of daily living and improve quality of life.
Neurologists are experts in designing comprehensive, patient-centered treatment plans, and are integral members of the care team. They utilize cutting-edge as well as time-tested treatments to maximize function and quality of life for their patients, who can range in age from infants to octogenarians.
We with our dedicated team of doctors give best service of rehabilitation to our patients so that they go back to their route job as soon as possible.
-
Dietary Services

Over the past century, deficiencies of essential nutrients have dramatically decreased, many infectious diseases have been conquered, and the majority of the indian population can now anticipate a long and productive life. At the same time, rates of chronic diseases—many of which are related to poor quality diet and physical inactivity—have increased. About half of all indian adult have one or more preventable, diet-related chronic diseases, including cardiovascular disease, type 2 diabetes, and overweight and obesity.
However, a large body of evidence now shows that healthy eating patterns and regular physical activity can help people achieve and maintain good health and reduce the risk of chronic disease.
We at our center have dedicated dieticians so that individually tailored advice is rendered to needy patients.
PHYSICAL MEDICINE & REHABILITATION
A series of dietary recommendations from the Nutrition Committee of the American HeartAssociation (and other bodies) intended to improve cardiovascular health.
Dietary Guidelines (American Heart Association)
- Caloric intake:
- Fat should be < 30% of total calories
- Saturated fat should be < 10% of total calories
- Polyunsaturated fat consumption should be < 300 mg/day
- Carbohydrates (especially complex type) should constitute 1/2 of calories in diet
- Protein should constitute the remainder
- Calories should be sufficient to maintain the body weight
- Sodium intake should be < 3 g/day
- Alcohol consumption should be ≤ 60 g (2 oz)/day1.
- A wide variety of foods should be consumed.
Segen's Medical Dictionary. © 2012 Farlex, Inc. All rights reserved.
Dietary guidelines
Cardiology A series of dietary recommendations from the Nutrition Committee of the AmHeart Assn, that promote cardiovascular health. See Caloric restriction, food pyramid, French paradox.
Dietary Guidelines-American Heart Association
- Fat should comprise < 30% of total calories
- Saturated fat should comprise < 10% of total calories
- Polyunsaturated fat consumption should be < 300 mg/day
- Carbohydrates (especially complex type) should constitute1⁄2 of calories in diet
- Protein constitutes the remainder, ie 100% – (1% + 4%)
- Sodium should be < 3 g/day
- Alcohol consumption should be ≤ 60 g (2 oz)/day
- Calories should be sufficient to maintain the body weight
- A wide variety of food should be consumed
- Caloric intake:
-
Botulinum Neurotoxin Type A at our clinic

Botulinum toxin (BT) is currently used in those entities characterized by excessive muscle contraction, including dystonia (like blepharospasm, cervical dystonia, linb dystonia, writers cramp), hemifacial spasm and spasticity (like post stroke spasticity). In addition, BT has been used to control pain associated with increased muscle contraction in dystonia and spasticity, but also is useful to control chronic pain not associated with muscle contraction, such as chronic daily headache. Finally, BT is useful in sialorrhea.
Neurological disorders that trigger spasticity as Stroke, Multiple Sclerosis, Head Trauma, Spinal Cord Trauma, Cerebral Palsy and some motor neuron diseases (Spastic Paraparesis, Amyotrophic Lateral Sclerosis), can be managed by applying botulinum toxin. The mechanism of action is complex, mainly acting on terminal neuromuscular junction, but also exhibiting analgesic properties, probably through inhibition of pain neurotransmitters release.